A High Price to Pay: Detention of Poor Patients in Burundian Hospitals
| Publisher | Human Rights Watch |
| Publication Date | 7 September 2006 |
| Citation / Document Symbol | A1808 |
| Cite as | Human Rights Watch, A High Price to Pay: Detention of Poor Patients in Burundian Hospitals, 7 September 2006, A1808, available at: https://www.refworld.org/docid/4517cb544.html [accessed 5 June 2023] |
| Comments | This 75-page report documents how Burundian hospitals in 2005 detained hundreds of indigent patients, sometimes in inhumane conditions. Many of those detained were women giving birth who unexpectedly needed caesarian deliveries. In some cases, hospital authorities refused further medical care to those who could not pay their bills and forced them to vacate their beds for wealthier incoming patients. |
| Disclaimer | This is not a UNHCR publication. UNHCR is not responsible for, nor does it necessarily endorse, its content. Any views expressed are solely those of the author or publisher and do not necessarily reflect those of UNHCR, the United Nations or its Member States. |
Acronyms
APRODH - Association for the Promotion of Human Rights and Detained Persons
CAM - Illness insurance card
CEDAW - Convention on the Elimination of all Forms of Discrimination against Women
CNDD-FDD - National Council for the Defense of Democracy-Forces for the Defense of Democracy
CNRS - National Commission for the Reintegration of the Displaced
EC - European Commission
ECHO - European Commission Humanitarian Office
EDF - European Development Fund
FBU - Burundian francs
FNL - National Liberation Forces
ICCPR - International Covenant on Civil and Political Rights
ICESCR - International Covenant on Economic, Social and Cultural Rights
MSF - Médecins Sans Frontières
ONUB - United Nations Operation in Burundi
PARESI - Project for the Support of the Repatriation and Reintegration of War Affected Persons
PRSP - Poverty Reduction Strategy Paper
UNDP - United Nations Development Programme
UNICEF - United Nations Childrens' Fund
WHO - World Health Organisation
I. Summary
I had to come to hospital because I needed a caesarean delivery. When I got the bill, the doctor said to me, "Since you have not paid, we will keep you here." Life here is difficult. I don't have permission to leave with my baby. We are often hungry here. I cannot stand this situation any longer.– Eighteen-year-old woman held with her baby at Louis Rwagasore Clinic, Bujumbura
One day, I tried to get out of the hospital and I was stopped because I had not paid my bill yet. When I see a doctor, I always ask to leave, since I am not getting any medical treatment.... The guards threaten me. Whenever I come near the exit, they tell me that I cannot leave because I have not settled the bill.
– Twenty-two-year-old man who had a car accident, held at Prince Regent Charles Hospital, Bujumbura
Hospital managers have to ensure financial stability. If the directors don't pay attention, they have to shut down the hospital.
– Dr. Julien Kamyo, chef de cabinet in the Ministry of Health
Over the past few years, public hospitals in Burundi have detained hundreds of patients who were unable to pay their hospital bills. Patients were routinely held for several weeks or months, and in one case for over a year. They were kept on the wards, guarded by security staff of the hospital, or were held in a separate room. Detained patients without money often went hungry if not fed by the charity of others. Some were forced to vacate their beds and sleep on the floor to make space for paying patients. Often, indigent patients did not receive further medical treatment once the bill had reached a large amount, even if they needed additional medical care, including basic follow-up care such as removing stitches after a caesarean delivery.
The detention of patients unable to pay their bills both results from and draws attention to broader problems of health care in Burundi. Although one of the poorest nations in the world, Burundi implemented in 2002 a cost recovery system as part of its delivery of health care services. The aim was to make the system more financially efficient. Patients must pay all medical costs, such as medical consultations, tests, medicines, supplies, and their stay at a hospital. There is a health insurance and a waiver system for the destitute, meant to assist the poorest in meeting medical expenses, but both function badly and in some places not at all. Public hospitals do not receive enough income from patient fees, direct donations and funds from the government to allow proper functioning, and they lack well-trained medical staff, equipment, and medicine. The Burundian health sector is plagued not just by huge funding shortfalls, but by inconsistent state funding, and by fraud and corruption that shrinks an already small pie. Hospital staff, who have been typically grossly underpaid, are among those involved in the financial mismanagement and corruption.
Most detained patients have had surgery, such as following an accident or as a result of birth complications, while others suffer from chronic diseases, including HIV/AIDS. The patients are very poor, often belong to vulnerable groups like orphans, widows, single mothers, or those displaced by Burundi's civil war, and lack family or larger networks of social support. Some of those detained are obliged to sell their last belongings in order to pay their bills and get released. Others find a benefactor (bienfaiteur), a wealthy individual or charity, to pay their expenses and allow them to return home.
On May 1, 2006, President Pierre Nkurunziza announced that maternal health care and health care for children under the age of five would henceforth be free of charge. If sustainable, this measure should end hospital detentions of some women and young children. However, it provides no relief for other patients unable to pay their bills who constitute more than half the persons typically detained.
Official responses to hospital detentions have been confused and contradictory, vacillating between denial, justification, and misrepresentation. Hospital managers and government officials often minimize the problem, claiming that those who cannot pay their bills are released after a few days. Most refuse to use the term "detention" to describe the practice. At the same time they justify the detentions as necessary, saying hospitals would be forced to close their doors if they could not use such means to oblige patients to pay their bills. Because government officials do not consider detention of patients to be a human rights violation, they take no measures to make hospital staff halt the practice, nor do they punish them for continuing it.
International human rights law provides that everyone has the right to liberty and security of person. Arbitrary detention of any kind is a violation of article 9 of the International Covenant on Civil and Political Rights (ICCPR), to which Burundi is a party. The detention of anyone for non-payment of a debt specifically violates ICCPR article 11, which states: "No one shall be imprisoned merely on the ground of inability to fulfill a contractual obligation." The detention in crowded conditions with scarce food violates the right of persons not to be detained under inhumane conditions.
Article 12 of the International Covenant on Economic, Social and Cultural Rights (ICESCR), to which Burundi is a party, requires states to progressively realize the right to the highest attainable standard of health. The detention of hospital patients who cannot pay their bills has important implications for health care in Burundi. Hospital detention discourages indigent people from seeking health care in the first place, subjects patients to having their treatment curtailed or ended when it is apparent to doctors and hospital staff that the patient cannot pay, and incarcerates recovering patients in conditions that may exacerbate their health problems.
The issue of hospital detentions also reflects the broader problem of access to health care for all members of Burundian society. While recent steps to end fees for maternity care and young children are welcome, the government should urgently provide health structures with the means to respond to the increased demands. More broadly, the government must ensure that funding for health care reaches the population most at risk, and take steps to reduce corruption in the health care system.
With the Millennium Development Goals, the international community has committed itself to reaching ambitious targets in the area of health, such as reducing child mortality, improving maternal health, and combating HIV/AIDS and malaria. In Burundi, international donors fund a large proportion of Burundi's health sector, and directly influence health policy decisions. Despite these commitments, donors have not pressed effectively for an end to the detention of patients, and for improved access to health care for the poor.
The Heavily Indebted Poor Countries Initiative might bring some change. Under this initiative, Burundi got debt relief on an interim basis during 2005, and the government has been able to almost triple the health budget as a result. The country is currently completing several economic measures, with a view to finalizing the debt relief agreement in late 2006. International financial institutions and other donors should ensure that such funds are used to improve access to health care and to end hospital detentions.
II. Recommendations
To the Government of Burundi
- Immediately effect the release of all current hospital detainees.
- Order an end to the practice of detaining insolvent patients in hospitals, and monitor hospitals to ensure that the practice does not continue. Take disciplinary or legal action as appropriate against persons responsible for hospital detentions.
- Propose legislation to make the detention of debtors, including insolvent patients in hospitals, illegal and punishable by law.
- Progressively implement the right to health by adopting measures to improve access to health care for the poor. Existing systems of cost exemption for the poor are inadequate and should either be reformed, or replaced with a new health care system. Reforms that should be considered include abolishing user fees for basic health care or the introduction of mutuelles, a community-based health insurance system. Any health policy reform should focus on access to basic health care for the poor and focus on the four essential elements regarding the right to health – availability, accessibility, acceptability and quality. In particular consider making health policy changes in the following areas:
- Urgently take measures to implement the new policy of free maternal health care and health care for children under the age of five. Ensure that primary health care systems are strengthened to respond to the increased demands, with access to staff, medicine, and equipment made available to all on an equitable basis. Develop a long-term plan on how to make this policy effective and link it with the broader health policy.
- Any future reform to abolish user fees should be prepared carefully as part of a larger policy, should rely on sufficient funding that is sought in advance, and should inform and involve stakeholders at all levels during the planning phase.
- Clarify plans to introduce a community-based health insurance and, if they are pursued, develop a strategy on how to include the poor in this scheme and ensure high levels of enrollment.
- Clarify plans to subsidize health care for the poor, as announced in the government health policy plan. Any cost exemption mechanism should be well publicized with clear criteria, administered in a transparent way, and include a patient's right to appeal decisions.
- Inform the public about ways to obtain assistance from the Support Project for Returnees (Projet d'Appui au Rapatriement et à la Réintégration des Sinistrés, PARESI) and from the Fund for the Displaced at the National Commission for the Reintegration of the Displaced (Commission Nationale pour la Réintegration des Sinistrés, CNRS), and any other cost exemption systems established.
- In the Poverty Reduction Strategy Paper (PRSP), lay out specific plans on how to end hospital detentions and reform the health system to improve access to basic health care for the poor.
To the newly established Government Anti-Corruption Brigade
- Investigate corruption in the health sector, including in hospitals and illegal sales of medicine, and ensure that those accused of crimes be promptly brought to trial according to international standards of due process.
To Donor Countries
- Urge the government of Burundi to end the detention of poor patients in hospitals immediately.
- Provide technical expertise to reform or replace existing cost exemption mechanisms and assist the government to develop health policy reforms that would better ensure access to health care for the poor, as outlined above.
- Provide positive incentives to the government of Burundi to dedicate a greater portion of debt relief funds to the health sector, particularly to improve access to health care for the poor.
- Ensure that development assistance for Burundi's health care system specifically addresses the problems of access to health care by the poor, which previously was funded through humanitarian assistance programs.
To The World Bank
- Urge that funds made available to the health sector through debt relief are used to end the detention of poor patients in hospital and to improve access to health services for the poor, including through health policy reforms, as those outlined above.
- Urge the government of Burundi to enforce laws on corruption and fraud and make use of the newly established government Anti-Corruption Brigade specifically to address misuse of funds in the health sector.
- Urge that development assistance for Burundi's health care system specifically addresses the problems of access to health care by the poor, which previously was funded through humanitarian assistance programs.
- Ensure that the PRSP and any future Poverty Reduction Support Credit (PRSC) for Burundi contain detailed plans for improving access to health care for the poor and fighting corruption in the health sector.
To the International Monetary Fund (IMF)
- Urge that funds made available to the health sector through debt relief are used to end hospital detentions and to improve access to health services for the poor, including through health policy reforms, as those outlined above.
- Ensure that the PRSP and any future Poverty Reduction Growth Facility for Burundi contain detailed plans for improving access to health care for the poor and fighting corruption in the health sector.
To the UN Special Rapporteur on the Right of Everyone to the Enjoyment of the Highest Attainable Standard of Physical and Mental Health
- Investigate the issue of detention of poor patients in hospitals in Burundi and other parts of Africa, and make recommendations to governments on how to end the practice.
III. Methodology
Researchers from Human Rights Watch and the Burundian Association for the Promotion of Human Rights and Detained Persons (Association pour la Protection des Droits Humains et des Personnes Détenues, APRODH) planned and carried out the research for this report. They interviewed 41 victims of hospital detention in six public hospitals: Prince Régent Charles Hospital in Bujumbura; Prince Louis Rwagasore Clinic in Bujumbura; Roi Khaled Hospital (the Centre Hospitalo-Universitaire de Kamenge) in Bujumbura; Gitega Hospital (Gitega province, central Burundi); Ngozi Hospital (Ngozi province, northern Burundi) and Muramvya Hospital (Muramvya province, central Burundi). They also interviewed hospital staff, including hospital directors, financial and administrative directors, doctors, nurses, and social workers. In addition, they interviewed representatives of local and international organizations working in the healthcare sector, public health experts, representatives of donor governments and agencies, and officials of the Ministry of Public Health and the Ministry of National Solidarity, Human Rights and Gender. APRODH observers interviewed hospital managers and others in five other hospitals in three other provinces (Karuzi Hospital, Muyinga Hospital, and Bururi, Rumonge and Matana Hospitals in Bururi province).1
We interviewed most patients when they were still in hospital detention, in February 2006. When citing the length of detention we generally refer to the amount of time the patient had been held at the time of the interview; we were not in a position comprehensively to monitor how much longer they may have subsequently spent in detention. Pseudonyms are used in this report for all hospital patients, to protect the identities.
Researchers also used quantitative data provided by the hospitals about the loss of income from insolvent patients. Although the format and detail of the reports varied significantly, researchers were able to analyze statistics from eight hospitals to determine changes over time, including, for example, the number of detained patients and the groups most commonly affected by detention.
IV. Background: Health, Poverty and Conflict
Political and socio-economic situation in Burundi: Moving from conflict to post-conflict
The current Burundian government under President Pierre Nkurunziza was elected in August 2005, following a decade of civil war and a long process of political transition. The dominant force in the government was formerly the country's largest rebel group, the National Council for the Defense of Democracy-Forces for the Defense of Democracy (Conseil national pour la défense de la démocratie-Forces pour la défense de la démocratie, CNDD-FDD). The CNDD-FDD portrays itself as a popular movement addressing the needs of the poor.
Another rebel movement, the National Liberation Forces (Forces de libération nationale, FNL), continued its war against the government, particularly in areas near the national capital Bujumbura. Both FNL and government forces continue to commit serious violations of international humanitarian law (the laws of war), including attacks on civilians.2 As of July 2006 the FNL and the government were engaged in peace talks.3
The long and violent conflict has had a destructive impact on society, the economy and the health sector. Burundi is now one of the least developed countries (LDC) in the world, ranking at 169 of 177 on the 2005 United Nations Development Programme's Human Development Index.4 The yearly gross national income per capita is at U.S.$90.5
The health sector in Burundi
During the period of armed conflict, health care deteriorated as shown by such key indicators as maternal mortality, infant mortality, vaccination rate and medical staff per inhabitant. Maternal mortality is at 1,000 deaths per 100,000 live births, and constitutes one of the most acute public health problems in the country, according to the World Health Organization (WHO).6 Infant mortality is at 114 per 1,000 live births (11.4 percent), and mortality of children under five is at 190 per 1,000 live births (19 percent) – these are among the highest in the world. The adult prevalence of HIV is 6 percent.7 The health system is plagued by a lack of trained staff and resources to pay them, as well as by a lack of medications and modern equipment.8 Many skilled medical staff leave the public sector in Burundi for better-paid jobs in international nongovernmental organizations (NGOs) or private health institutions, or in neighboring Rwanda.9
Access to health care was made more difficult for poor Burundians by the adoption of a cost recovery system in February 2002. Patients, regardless of their means, must pay all medical costs, such as medical consultations, tests, medicines, supplies, and their stay at a hospital.10 Only five of seventeen provinces operate alternative models of health financing.11
The cost recovery system revived a health policy from before the war that had not been properly put into practice. Before the 1980s, health care services were free of charge in Burundi. In 1988, the government started a policy of reform and decentralization: It introduced a pre-payment system at the community level and established management autonomy in the health structures at the provincial level, which meant that hospitals were running their operations with a degree of independence (autonomie de gestion) and were obliged to raise some of their funds themselves, while still receiving some state subsidy.12 The 1988 reform also aimed to gradually implement a cost recovery scheme in all health structures, but was halted during the following decade of armed conflict.13
Health policies in Burundi are partly the result of the government's own priorities: the government devotes only a small fraction of the budget to health – in 2005 just 2.7 percent.14 They are also the result of the World Bank's policies across Africa during the 1980s and 1990s, which intended to bridge a "health sector resource gap" through user fees. The strategy was given added weight by the Bamako Initiative, developed by the WHO and UNICEF and adopted by African governments in 1987. 15 The Bamako Initiative aimed at improving access to primary health care through involving communities in managing and financing health care. It was hoped that cost recovery at the community level would increase the revenue of the health sector, promote an efficient use of resources, and increase equity – that is, overcome differences in access to health care.16 The introduction of user fees was seen as a step towards rebuilding a sustainable health care system, including in countries wrecked by armed conflict.17
Studies show that the cost-recovery initiatives for health financing rarely had the desired impact. Cost recovery systems in Africa raised less revenue than expected, and there is little evidence that they improved the efficiency of health care systems.18 In Burundi, access to the health system is limited, with about one million people – 17 percent of the population – being excluded from health care altogether.19 Because of this limited access, hospitals have a low occupancy rate, despite the enormous needs of the population.20 The World Bank no longer promotes cost recovery as the sole option, and donors have moved to a more nuanced position.21 Yet, cost recovery is still the most common health financing model in Africa.
Several mechanisms were meant to ease the pressure on the poor in Burundi, but have failed to do so: the indigence card (carte d'indigence),which waives health fees for the very poor; a voucher that waives health fees for displaced people; and the illness insurance card (carte d'assurance maladie, CAM), which can be bought for the equivalent of about $0.5022 and reduces the medical bill by 80 percent. Both in Burundi and elsewhere in Africa, such programs have rarely been effective in expanding access to health care.23
Availability and access to health care
Burundi is a relatively small country and 80 percent of the population lives within five kilometers of a health center.24 Still, transport – particularly prompt transport – to a health facility poses a problem for those lacking money. For example, 39-year-old Michelle N. could not get transport when she went into labor at night. She lives in Gatumba, about six miles from Bujumbura. She was able to reach the hospital only at 5 a.m. the next morning, by which point her baby had died. She was then unconscious for two days.25
Some patients seeking help find that the nearest facility lacks the staff or equipment needed for appropriate care, and must move on to another hospital.This was the case of 13-year-old Noah B., who injured his ankle while playing football. His father took him to the nearest hospital, at Kayanza, only to be told that the hospital could not perform the surgery Noah needed. They borrowed money for a taxi to Roi Khaled Hospital in the capital.26 Many women in labor whom we interviewed during or following hospital detention were also sent from one hospital to another. Researchers interviewed one woman who while in labor had gone to four health facilities before being admitted.27
The poor may confront the further obstacle of lacking money to pay the fee for admission to a hospital. Most hospitals require patients to pay fees before receiving care. Fees vary according to hospital and according to the evaluation of the case, with large hospitals in Bujumbura charging the equivalent of approximately $10 for simple cases and up to $100 for more complicated cases or ones where surgery will be required.28 Outside the capital the admission fees are lower. At Ngozi hospital, for example, the regular admission fee is approximately $5.29 Anne K. is a woman who could not pay the admission fee at Prince Régent Charles Hospital in Bujumbura at the birth of her second child:
For medical reasons, I cannot give birth normally, so I must have a caesarean delivery. At the birth of my first child, I found a benefactor who took me to the MSF [Médecins Sans Frontières] clinic and I had a caesarean delivery there. This time there was no benefactor. I went to Roi Khaled Hospital but they refused to admit me because I had no money to pay the admission fee. They sent me to Prince Louis Rwagasore Clinic. There, they were reluctant to do the caesarean delivery so soon after the first one. So I went to Prince Régent Charles Hospital. They, too, refused me because I had no money. I thought to myself, "There is nothing else I can do. If I have to die, I will die." I left, but then the doctor ran after me and said, "I will do it."30
As the example of Anne K. shows, some persons needing care were admitted even if they lacked money to pay the admission fee. Such decisions, however, were the exceptions to the usual rule. Gabriel N., a man who suffered two road accidents, was also rejected because he could not pay the admission fee:
On November 22, 2005, I came here to the hospital [Roi Khaled]. The doctors refused to treat me because I could not pay the admission fee. I stayed outside the hospital for a few days, trying to get treatment. One day a man passed by and asked me why I had been there so long. I explained my problem and showed him my injury and he paid the admission fee of 100,000 francs [FBU, $100].31
Getting admitted to a hospital is by no means the same as getting medical treatment. Burundi's hospitals are poorly equipped and staffed, and medical care is often insufficient or inappropriate.32
Hospital detentions in Africa
The detention of poor patients by hospitals is found in numerous other African countries where the health system is based on a cost recovery system and hospitals try to force insolvent patients to pay their bills. The practice is found in countries including Kenya, Ghana, the Democratic Republic of Congo (DRC), and there has been at least one instance in Zimbabwe, affecting multiple patients.
Wealthy patients in Kenya can get private health insurance, high quality medical treatment and hospital accommodation, but most Kenyans cannot afford such insurance and are relegated to substandard hospitals where they have to pay for services and end up detained if they fail to do so.33 In Ghana, women who have delivered babies are frequently kept in the hospital until they pay the costs for childbirth. The country is in the process of introducing a flat fee for poor and vulnerable patients but this will not cover high-cost surgery including caesarean deliveries.34 In the DRC, a local human rights organization focused on the situation of young mothers in hospital on International Women's Day 2006, showing both the growing frequency of detentions of women in hospitals and their rejection by family members who do not want to be forced to pay for them. Among the detained women are rape victims who are completely isolated and unlikely to find anyone to pay for them.35 The detention of patients is not the rule in Zimbabwe, but in one case, 28 mothers and their newborn babies were detained at Harare Hospital. The charges for maternal health care had just risen and the women were unable to pay the bills for childbirth.36

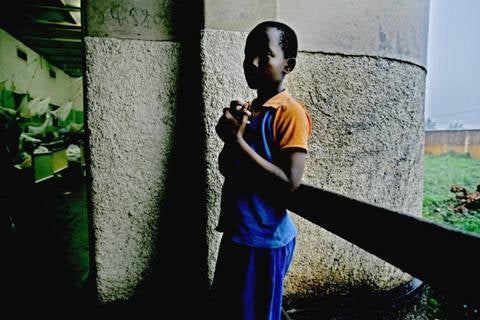
A young mother and her newborn baby, detained at Prince Louis Rwagasore Clinic following a caesarean section.© 2006 Jehad Nga
V. Detention in Public Hospitals for Lack of Payment
Numbers of hospital detainees
Statistics kept by Burundian hospitals show that they have been struggling with the problem of unpaid bills for years, and that the detention of patients is not a new or ad-hoc measure.37 Hospitals short on funds began detaining patients unable to pay their bills in the 1990s,38 when cost recovery was already practiced in some health facilities, and have done so with increasing frequency since the wholesale introduction of the cost recovery system in 2002.
During 2005 hundreds of patients were detained in Burundian hospitals. Data from seven of the thirty-five public hospitals in Burundi combined show 1,076 cases of patients who were unable to pay their bills in 2005 (see table 1). This figure includes both those who were detained and those who managed to leave without paying their bills. Given that this sample represents only a fifth of the public hospitals in Burundi, the total number of patients unable to pay their bills was certainly far higher. At the Prince Régent Charles Hospital alone, 621 patients were detained during 2005. Of those, 354 patients had their bills eventually paid by benefactors, and the other 267 found a way to leave the hospital without paying.
Figures on unpaid bills at Roi Khaled Hospital show varying numbers since 2001 (see table 2), with an average shortfall of about U.S.$39,000 per year. At other hospitals, similar figures are not available, but there are statistics documenting the loss of income in 2005 (see table 3). At Prince Régent Charles Hospital, staff have also documented a steep rise in the number of bills paid by benefactors: a total of 44 for the three years 2001-03; 85 in 2004 alone, and 352 in 2005.39 It can be assumed that in most cases benefactors paid bills of patients who were unable to pay their bills and had been detained. It is likely that the rise represents a real increase in the number of hospital detainees, though other factors – such as increased media attention to the problem – might have exaggerated this trend. 40 Statistics of the much smaller Prince Louis Rwagasore Clinic show an increase in the number of indigent persons listed in their books: 11 in 2001, 18 in 2002, 16 in 2003, 16 in 2004, 39 in 2005 (table 4).
Table 1
Number of patients who did not pay their bills at seven Burundian hospitals in 2005
| Roi Khaled Hospital, Bujumbura | 42241 |
| Prince Régent Charles Hospital, Bujumbura | 26742 |
| Ngozi Hospital, Ngozi province | 217 |
| Bururi hospital, Bururi province | 36 |
| Hôpital de Rumonge, province de Bururi | 36 |
| Hôpital de Matana, province de Bururi | 51 |
| Hôpital de Muramvya, province de Muramvya | 47 |
| Total | 1076 |
Table 2
Unpaid bills at Roi Khaled Hospital, Bujumbura, 2001-2005 (FBU) (1,000,000 FBU = approximately U.S.$1,000)43
| 2001 | 2002 | 2003 | 2004 | 2005 |
| 23,334,446 | 64,150,549 | 34,297,612 | 25,666,425 | 47,769,382 |
Table 3
Unpaid bills at seven hospitals44 in 2005 (FBU)
| Roi Khaled Hospital, Bujumbura | 47 769 382 |
| Prince Régent Charles Hospital, Bujumbura | 24 498 99245 |
| Ngozi Hospital, Ngozi province | 9 492 170 |
| Bururi Hospital, Bururi province | 1 115 050 |
| Rumonge Hospital, Bururi province | 2 174 350 |
| Matana Hospital, Bururi province | 460 540 |
| Muramvya Hospital, Muramvya province | 2 270 351 |
Table 4
Indigent46 patients and their bills at Prince Louis Rwangasore Clinic, Bujumbura, 2001-2005 (FBU)
|
2001 |
2002 |
2003 |
2004 |
2005 | |
| Number of indigent patients |
11 |
18 |
16 |
16 |
39 |
| Bills by indigent patients |
1,716,744 |
1,753,456 |
2,568,408 |
2,586,682 |
7,629,331 |
Medical problems leading to detention
Data from four hospitals show that during 2005, surgical patients represented about two-thirds of all indigent patients. The remaining one-third of indigent patients were mostly from two types of ward: internal medicine (16 percent) and pediatrics (10 percent). Of indigent patients overall, 35 percent were women who had delivered their babies by caesarean section.47
Surgery
It is not surprising that many victims of hospital detention were patients who had undergone surgery, given that surgery is often more expensive than ordinary medical care. In addition to women undergoing caesarean deliveries (discussed below), we interviewed several men who had suffered bad road accidents, a woman with breast cancer, and the mother of a baby who needed urgent surgery on the intestines.
Félix M. has been in detained in Prince Régent Charles Hospital for over one year, after having already spent a year there for treatment. The thirteen-year-old boy was hit by a vehicle when he was playing with other children. He suffered a serious leg injury and underwent surgery. His father allegedly embezzled the insurance funds destined for his hospital care, and his mother had been unable to find a way to pay for the treatment. As of August 2006, Félix M. continued to be detained.
© 2006 Jehad Nga
Patients suffering from long-term or chronic diseases, including HIV/AIDS
Patients with long-term or chronic diseases also incurred high hospital costs that they could not pay and that resulted in their detention. People with chronic conditions are often unable to work and therefore depend on others to pay their hospital bills. One such example was Christian B., an 18-year-old young man who suffered from a serious skin disease. He was an orphan, and the uncle who was looking after him could not pay his hospital bill. He said local authorities refused to issue an indigence card for him, saying the card was not being used any more.48 Christian B. told us,
I have had a skin disease for about two years now. I went to Bujumbura for treatment but they refused to treat me, so I came here. I was given medicine at the hospital and it got better. I was put in an isolated room. I could not pay the bill but around Christmas 2005 I was released along with other people. I had a bill of over 240,000 FBU [$240]. Now the illness has come back. I came back to the hospital.49
There are about 220,000 people50 living with HIV/AIDS and 46,000 people in need of AIDS treatment in Burundi, and many of them also face detention in hospital.51 The Global Fund to Fight AIDS, Tuberculosis and Malaria is currently providing about $21 million to the Burundian government for treatment and prevention. Under this program, antiretroviral drugs are provided for free.52 The World Bank runs a multi-sector program on HIV/AIDS in Burundi of $36 million over a period of four years.53 But even with this level of international assistance, only about 6,400 persons received the life-saving drugs without cost in 2005, while about 40,000 more needed the drugs but were unable to benefit from them due to the inaccessibility of treatment sites and other reasons.54 Many of those without antiretroviral drugs seek medical care for opportunistic diseases such as tuberculosis, pneumonia, fungal infections or other diseases, and they usually have to pay for treatment.55 According to the medical director in the Ministry in Charge of the Fight against AIDS, around 70 percent of internal medicine patients have HIV/AIDS.56 Records of four hospitals show that about 15 percent of all indigent patients in 2005 were internal medicine patients (see table 5).
Because of reluctance to discuss AIDS and absence of any indication on hospital records, we collected no data on the frequency with which AIDS patients were detained for unpaid bills.
We spoke to one patient who identified herself as suffering from AIDS. She was detained for two months for failing to pay for treatment for a fractured arm and leg.57
Table 5
Number of patients unable to pay their bills58 by ward (medical department) in 2005
| Roi Khaled Hospital, Bujumbura | Prince Louis Rwagasore Clinic, Bujumbura | Prince Régent Charles Hospital, Bujumbura | Muramvya Hospital, Muramvya province | |
| Total | 422 | 39 | 267 | 47 |
| Gynecology/ Obstetrics | 91 | 24 | 137 | 15 |
| Surgery | 100 | 6 | 47 | 13 |
| Internal Medicine | 64 | 1 | 42 | 14 |
| Pediatry | 48 | 4 | 22 | 3 |
| Intensive Care and Emergency | 46 | 1 | 6 | 0 |
| Operating theatre (anaesthetics etc.) | 64 | 3 | 5 | 2 |
| Other | 9 | 0 | 8 | 0 |

This newborn boy urgently needed surgery after birth. As the mother could not pay for it, she and the baby got detained at Roi Khaled Hospital.
© 2006 Jehad Nga
Maternal health problems before May 1, 2006
Before the presidential order on maternal and child health care on May 1, 2006, a significant proportion of hospital detainees were women who had suffered complications in connection with the birth of a child, such as those who delivered by caesarean section.
While 35 percent of indigent patients unable to pay their bills were women who had recently given birth, the situation varied considerably by hospital.59 At the time of one visit to Prince Louis Rwagasore Clinic to research this report, in February 2006, all the detainees were women who had delivered by caesarean section, and according to the guards, this was often the situation.60
At 1,000 deaths per 100,000 live births, the maternal mortality rate in Burundi is alarming. About 80 percent of deliveries take place at home without the assistance of a trained health professional.61 There is no functioning referral system that ensures timely access to hospitals in case of complications. Emergency obstetric equipment is not available as widely as it should be. Research has shown that lack of access to emergency obstetric care is one of the main causes of maternal mortality worldwide.62
Infant and child health problems
Another important group among those detained – about 10 percent – were infants and children. As mentioned above, infant and child mortality rates in Burundi are among the highest in the world. This is due in large part to malaria, diarrhea, pneumonia, and HIV/AIDS.
Malaria is responsible for 50 percent of hospital deaths of children under age five. Acute respiratory illness and diarrhea are also frequent causes of death in young children, mostly due to the lack of potable water, inadequate sanitation, and poor housing conditions. About 44 percent of children are malnourished or stunted, and 56 percent suffer from anemia. Approximately 27,000 children under the age of fifteen have HIV/AIDS. Immunization rates for the deadliest childhood diseases have declined in recent years.63 Experts have found that about two-thirds of child deaths could be averted if proven existing health interventions could be made available.64
The introduction of free health care for women giving birth and children under five constitutes an important step towards improving maternal and infant health, and ending detention among patients of this vulnerable group.

A young mother and her newborn baby, detained at Prince Louis Rwagasore Clinic following a caesarean section.© 2006 Jehad Nga
"Since you have not paid, we will imprison you": Experiences of patients
The moment when hospital staff hand patients their bill can mark the transition from hospital treatment to hospital detention. Hospital staff – mostly nurses and doctors – impose the detention and attempt to justify it to the patients. Hospital managers – medical doctors as well as administrators – also justified the detention to Human Rights Watch researchers.65 Hospital staff may detain patients because they believe it is necessary in order to keep the hospital functioning. Nonetheless, in doing so they violate their own ethics66 and their conduct leads to a breach of trust in a privileged relationship. They also become agents of a human rights abuse.
Christine K., an 18-year-old who gave birth by caesarean section, recounted her experience. At the time of the interview she had been three weeks in detention. She said,
When I got the bill, the doctor said to me, "Since you have not paid, we will imprison you." Life here is difficult. I don't have permission to leave with my baby. We are often hungry here. I cannot stand this situation any longer. 67
Pierre B. is a middle-aged man who was hit by a car when walking home after church service in November 2005, and held for one month at Prince Régent Charles Hospital when we spoke to him. He explained,
My leg and face were crushed. I was unconscious for one day. In January, I was given a bill of 205,445 [FBU, $205]. When I said that I cannot pay this, I was told to stay.68
Josephine C., whose baby was sick, tried to plead with the hospital director for her release but he only confirmed her detention:
I spoke with the director of the hospital and I told him that I couldn't pay. He said that I cannot leave the hospital, that I have no right to leave the hospital until I paid the bills.69

A young mother and her newborn baby, detained at Roi Khaled Hospital following a caesarean section.© 2006 Jehad Nga
Some patients, such as Josephine C., knew about the risk of detention. Other patients were caught off guard by the high costs of their treatment. Claudine N., an 18-year-old mother of two, did not expect a high bill for the delivery of her baby. At the time of the interview, she had been held for six weeks:
I got the bill on December 28, 2006, and it was over 116,000 FBU [$116]. I did not expect that because Roi Khaled is a public hospital. The doctor said to me, "We cannot do this differently, you have to stay here."70
The length of detention of patients varied greatly, depending in part on whether the patient can find a benefactor to pay the bill or find a way to evade surveillance and leave. Most patients interviewed were detained for a period of several weeks or months, but a few were kept for about a year.
Surveillance
In most hospitals, detained patients are able to move around the building but are prevented from leaving the premises by security guards from private security companies contracted by the hospitals.71 According to several patients, security guards on the grounds generally knew the names and faces of those detained, often because they had been pointed out to them by hospital staff. Several detainees said guards followed them around even within the hospital premises.72 As a consequence, patients could not leave even for a moment, unless they got express permission to do so. As one victim put it, "I am detained because I cannot pack up my things and leave. To leave means to escape."73
Théodore N. was detained for two weeks in Prince Régent Charles Hospital after he received treatment for an accident injury. He told us,
I am really imprisoned here. One day, I tried to get out of the hospital and I was stopped because I have not paid my bill yet. When I see a doctor, I always ask to leave, since I am not getting any medical treatment. The guards threaten me. Whenever I come near the exit, they tell me that I cannot leave because I have not settled the bill.74
Patients in other hospitals had similar experiences. A patient who was held for three months in Gitega Hospital complained that whenever he would leave his bed to sit in the sunshine, guards or other hospital staff would come and ask him where he was going.75

A patient detained at Prince Régent Charles Hospital. © 2006 Jehad Nga
At Ngozi Hospital, the director of finance and administration explained how surveillance by a private security company is essential. Either patients stay until they find someone who pays, or – if they flee – the company pays a fine. Because of the large numbers of people escaping, the hospital has negotiated a modus vivendi with the security company, reducing the fine to a sum that is acceptable to them:
We have come to an arrangement with the security company. For us, [using the security company] is a way of cutting down on the costs. Otherwise the hospital would have to be shut down.76
Seventeen-year-old Félicité G. had been held for two weeks at Ngozi hospital when she spoke to us. She described what surveillance meant for her:
I am detained because I cannot gather the money to pay the bill. I cannot leave or move around. I am watched everywhere because they always think I want to escape. But it is not good to run away. When they catch you, you cannot go back for treatment. I would be punished for that.77
Other detainees in Ngozi and elsewhere confirmed that they did not escape because they feared that they or their children might fall ill at some future time and be refused treatment.78 They preferred to stay detained in the hospital than to risk having no possibility of hospitalization during the next illness.
Nevertheless, some patients found ways to leave hospital. At Prince Régent Charles Hospital, 191 did so between January and August 2005. Many left at night, and one person had left disguised in the clothes of a Muslim woman.79 According to one patient, two persons caught trying to leave surreptitiously were mocked and insulted by nurses.80
Prince Louis Rwagasore Clinic: Detention in a lock-up
Detainees at Prince Louis Rwagasore Clinic are held in a separate room with a guard at the door and are not allowed out of the room. When visited by researchers on February 14, 2006, about 20 people were in the room, about a dozen mothers with newborn babies who were confined there, plus some family members who were assisting or visiting them. A filthy toilet and shower constituted the sanitary facilities for all the detainees and visitors.
Agnès I., a 23-year-old woman who delivered her baby by caesarean section on January 17, 2006, could not pay her bill equivalent to $235 and so was moved to the lock-up, where she had stayed for one month when we spoke to her. She said she was told to stay in the room until she found money or a benefactor. She continued, "I have tried to get the money together but I have not managed. I stay here, I cannot get out. I cannot even go out to dry the clothes I have washed."81
According to those guarding the room, most detainees were women who had had birth complications. Many were held until the babies were able to hold up their heads, meaning two or three months. When patients left without paying, the guards sometimes followed them home.82

At Prince Louis Rwagasore Clinic, detainees are held in a separate room with a guard at the door. At the time of our visit, the room held about twenty people. The sanitary conditions in the room were deplorable: there was a filthy toilet and a shower, and they could not be used in private because they belonged to the room. One person who had been held for a month, said: "After I got the bill I was directly taken here and told 'Stay here. When you have money or there is a benefactor, you can leave.'" © 2006 Jehad Nga
Size of bills
Bills vary in size according to the services received by the patients. Even amounts that seem relatively small may exceed the monthly income of a poor Burundian. Félicité G., a 17-year-old mother, was held at Ngozi Hospital because she could not pay the equivalent of $9 for the treatment of her baby, who was sick with malaria.83 At the opposite extreme, David S. from Rutana province was hospitalized after he had a bicycle accident, and now faced a bill equivalent to $1,750, an enormous sum by the standards of ordinary Burundians. He said,
We arrived in Gitega hospital on June 15, 2004. At that moment I had nothing because the rebels had come to my house and looted almost everything. I was operated [on] here, but there was no improvement. Three months ago, they came to see me and told me to pay... 1,750,000 FBU [$1,750]. I don't see how I can pay this bill, because I do not even have a plot of land that I can sell.84
When the bills are very high, it is harder to find benefactors. Therefore, patients who have had costly surgery or other expensive treatment are likely to be held for longer.
Conditions of detention
Lack of medical treatment
Hospital officials sometimes refuse further treatment to patients who have shown themselves unable to pay the cost of their medical care. At Prince Louis Rwagasore Clinic two young mothers who were detained following caesarean deliveries asked medical staff to treat their newborn babies, who had respiratory problems and were vomiting. According to the women, the staff refused. They said that doctors and nurses never entered the lock-up at Prince Louis Rwagasore Clinic.85
Michelle N., whose case was mentioned earlier, gave birth to a stillborn baby at Prince Régent Charles Hospital and was unconscious for two days after the birth. When she could not pay the bill she was moved to ward nine where many detainees were kept, and where she stayed for about ten weeks. There was no assistance from medical staff:
I got a fever and asked for treatment, but it was refused. The nurse said that I would have to pay the 10,000 FBU [$10] admission fee to obtain the registration form. Luckily the fever went away.86
At Gitega Hospital, nurses allegedly went one step further and refused to remove the stitches that closed the incisions from caesarean deliveries. If stitches are not removed, the incision may get infected. Emérite N., a poor farmer from Mwaro province, gave birth at Gitega hospital to a child who died after two weeks. In addition to coping with her grief, she was overwhelmed by a bill equivalent to $45 that she was unable to pay. She said, "I was told that they cannot remove the stitches until I have paid the bill. The stitches are now hurting. I worry that I will get an infection, and I feel trapped here."87
Sometimes hospitals also refuse to carry out treatments on patients who will be unable to pay the costs, probably because they want to avoid expenditures which they will not be able to recover. Dorothée H., a widow who had recently returned from living as a refugee in Tanzania, was taken in by a family in Bujumbura and survived by selling tomatoes. She had the misfortune to fall and break her hip but did not seek treatment immediately. When her condition worsened, she said she went to two private clinics where she was refused, at the second one because she lacked the equivalent of roughly $100 needed for the admission fee. She entered a public hospital where doctors did some tests and advised surgery to replace her hip. Since the cost would be $400, clearly beyond her means, the surgery did not take place. Unable to pay her bill, even without the surgery, she remains in the hospital where she can hobble only a few steps at a time with the help of a cane.88
Lack of food
Almost all detainees complained of hunger. Hospitals in Burundi generally do not provide meals to patients, who depend on family members, charities or benefactors to give them food and drink. Human Rights Watch observed that those detained were particularly affected, due to their indigence and the length of their stay at the hospital, and those who had no family members nearby and willing to help or who did not find assistance elsewhere just went hungry. Agnès I., a young mother who had undergone a caesarean delivery, said that her relatives only rarely brought food and that patients had to buy even the water needed to make coffee or tea.89 Another young mother who had been detained for two months at a different hospital said, "For me it is difficult to get food. My family is tired of bringing food here. I have not even had tea today. I am waiting for God's help."90
In some hospitals, nuns provided food once a day to detainees who were grateful but pointed out that the food was of poor quality and insufficient in quantity, in particular for patients recovering from illness or surgery.
Losing the bed
Sometimes detained patients had to vacate their beds for patients who could pay. Gabriel N., mentioned above, told us after five weeks of detention at Roi Khaled Hospital:
I feel like I am in a prison here. I lost my bed last night to a sick person who could pay. So I slept on the floor. I don't know when I will have another bed. They promised me that when a sick person leaves, I will get a bed.91
Several detained persons in Ngozi Hospital complained of the same practice.92 Christian B., the young man with a serious skin disease, mentioned above, who was hospitalized at Nogzi for about six months in 2005, was detained for non-payment of a bill of over $240. He reported having to sleep on the cement floor when paying patients arrived needing a bed.93 Also in Ngozi Hospital in March 2006, four other detained patients had been obliged to vacate their beds. One was a 65-year old widow. Two others were 17-year-old Félicité G. and 20-year-old Valentine Z., both of whom were sleeping on thin mats on the cement ground with their babies.94
Children in hospital detention
Children are not spared from hospital detention. Mothers stay with babies and small children while older children are sometimes held by themselves, with little or no support from the hospital.95
Mohamed S.
Three-year-old Mohamed S. was burnt badly all over his body when he was playing with other children and they accidentally tipped over a pot of boiling beans. At the time he was visiting his grandmother, who took him to hospital and had stayed with him since. They arrived at the hospital on November 16, 2005, and were detained for about six weeks when they spoke to us. Mohamed's grandmother told us,
I received a first, incomplete bill at the end of December. It was not complete because they continued treatment. I was afraid of seeing it. It was more than 400,000 FBU [$400]. I have asked for the final bill because I am worried about the amount of money. We have been told we are not allowed to leave, even though the boy is now healed.96
The situation has been particularly difficult for the grandmother because her son, the child's father, holds her responsible for the accident and refuses to provide money for the hospital costs.

Three-year-old Mohamed S. was burnt badly all over his body when he was playing with other children and they accidentally tipped over a pot of boiling beans. At the time he was visiting his grandmother, who took him to the hospital and stayed with him since. When we met them, they had been detained in Roi Khaled Hospital for six weeks. Mohamed's grandmother, who can be seen in the background, explained: "We have been told we are not allowed to leave, even though the boy is now healed." © 2006 Jehad Nga
Noah B.
Thirteen-year-old Noah B. was injured while playing football with his friends. He broke some bones in his ankle and needed surgery. He is one of eleven children and his parents are farmers. His mother and siblings stayed in their home province of Muramvya while Noah's father accompanied him to Roi Khaled Hospital in Bujumbura and took care of him there during the treatment and the detention that followed. At the time of the interview, Noah B. had been held for about six weeks. His father told us,
We owe 438,785 FBU [$438] for Noah's surgery. We are waiting for a benefactor because we will never have that much money.... The situation now is very hard. I have pretty much abandoned my house because I have spent all my time here. I have two younger children at school but I had to abandon everything and leave it all behind to be in the hospital with Noah.I am free, I can come and go from this hospital, but my son cannot leave. He cannot escape. The doctors threaten us, telling us that soon Noah will lose his bed and will have to sleep on the floor so that a paying person can have the bed.97
Noah told us that he was in his first year of school when the injury happened, and that he wants to return to school as soon as possible.98
Félix M.
Félix M., aged 13, has been detained at Prince Regent Charles Hospital for over a year, after having already spent a year there for treatment for injuries suffered when a vehicle belonging to the African Union mission in Burundi struck him in July 2004. His father spent or used the money provided by the United Nations Operation in Burundi (ONUB), the successor agency to the African Union, for the boy's care. His mother, who struggled to find the money necessary to pay just for Felix's medicine, was unable to find a way to pay the rest of the hospital charges. Felix said,
I was in seventh grade in school but now I am not going to school any more. Now I am healed, there is just one small injury left. My family cannot pay the bill. I have been told that I cannot leave unless the bill is paid. I am detained here because I cannot go past the exit. The nuns give me food twice a day.99
The truth of Felix's predicament emerged as a result of research done for this report.100 Although Felix's father admitted to taking the money, he had nothing left of it.101 As of August 2006, Felix was still detained at the hospital.
Adèle A.
Twelve-year-old Adèle A. from Cibitoke province suffered a broken leg in an automobile accident in January 2006 when returning home from school. Following surgery, she had been detained for over four months at Prince Régent Charles Hospital when we interviewed her. She said,
I have no father and my mother is a farmer. My mother stays with me in the hospital here and tries to find things for us to eat. It is very hard. We have no family here, everyone is back in Cibitoke. We have no land so we cannot sell anything to pay the bills. Even to cultivate crops, we rent a plot. Right now, I have my bed but I am afraid that I will lose it. The conditions here in the hospital are very difficult. Sometimes I go for two weeks without soap... No one told me that if I couldn't pay, I would have to stay in the hospital. It's just accepted as normal that you just cannot leave if you haven't paid the bill.102
Refusal to release dead bodies
When patients die and medical bills have not been settled, hospitals frequently refuse to hand over the bodies to family members. As a burial according to Burundian tradition becomes impossible, it is hard for mourners to express their grief in culturally acceptable ways. Francine U. died in December 2005 of malaria during pregnancy. The nurse at Roi Khaled Hospital who cared for her said:
She came too late, and she died. Her brother was with her but he left when she died. He did not pay her bill so her body stayed in the morgue. She is still there.103
The nurse confirmed that bodies are often held in the morgue for long periods if relatives cannot pay the bills, but said that if there are bodies at the morgue for a very long time, eventually "the hospital management will deal with it and bury them."104 According to research by APRODH, there were seven bodies held at the morgue of Roi Khaled Hospital in August 2005. The relatives of the deceased had not paid the bills, which totaled more than $1,400.105
VI. Consequences of Hospital Detention
Economic pressure
Large hospital bills often have disastrous economic and social consequences for the recipients and their families. If patients are detained, the pressure to pay the bill increases and their ability to earn the money to pay the bills decreases. A study by Save the Children found that if poorer households managed to pay for health care, more than half of them did so by selling assets. Another 20 percent borrowed money from a friend or relative. The study concluded that these are "risky, irreversible strategies" that are "potentially catastrophic" for households that are already poor.106 A larger study by Médecins Sans Frontières Belgium reached similar conclusions, finding that more than 80 percent of the households surveyed paid for healthcare by incurring a debt, selling a possession (cattle, land or harvest) or by taking on additional work, for example agricultural labor.107
In seeking release of themselves or family members from detention by selling such resources as land or cattle even though they need them for their livelihood, people are drawn deeper into poverty.108 The situation is particularly difficult for those who have few social networks, such as orphans, widows or returnees, and hence few possibilities of getting help. Gabriel N., the man who suffered two road accidents, told our research team,
I had a wife, but since my accident, she went back to her parents. I am an only child and an orphan. My parents died when I was very young. My wife tried to help me with the medical bills, but when she had nothing remaining, she left me. I am just a farmer and I have only once piece of land. I do intend to pay these bills and if I could leave here, I might be able to start to pay things back. I think that my best option would be to sell my land, because otherwise, I will never be able to pay the hospital bills. If I could work, I could earn money, but I need to be in good health. This is my dilemma, I am not sure if I should sell my land and abandon my parcel or if I should stay here and wait for a benefactor.109
The father of Noah B., the boy detained following surgery on his foot, also faced serious economic hardship:
My land is all I have. Even if I sell the land, it won't cover the cost of the medical expenses. I had a cow, but it was stolen during the war. If I still had the cow, maybe I would have others now and we would have more money. My nephew used to help me work on the land and lend us money, but he was killed three weeks ago by bandits in Bukeye. My wife is trying to manage. I sell bananas sometimes and occasionally manioc flour to make a little money.110
Women and children often do not have legal access to property and cannot take decisions about the sale of land or other property without the approval of a male family member. Male heads of household control family resources, and women and children may have no information about the family's financial situation, including whether there is in fact the means to pay the hospital bills. This helps explain the case of Félix M., described above, whose father stole the money that had been supplied by ONUB and that was meant to pay his hospital bill.
Detained children such as Noah B. and Félix N. miss out on schooling. For some, their forced stay at the hospital is likely to have a negative long-term effect on their education and consequently their livelihood prospects.

A boy detained at Roi Khaled Hospital. His father, who is a farmer and cannot pay the bill for surgery, is staying with him. © 2006 Jehad Nga
Fear to seek access to health care
In addition to economic consequences, detention shatters the trust of individuals detained, and others, in the health system. As knowledge of the practice becomes generally known, fear of detention may result in individuals delaying seeking care or avoiding it altogether, or going instead to a traditional healer. Josephine C., whose baby was sick, initially avoided going to hospital because she expected to be detained:
I would be kept there for a long time because I wouldn't be able to pay the bills. But I didn't have a choice in the end. I was already here in Bujumbura when the baby got really sick and so I finally came to the hospital here.111
Olivia N., who suffered from long-term birth complications, also delayed her trip to the hospital as long as possible:
I had complications after having a baby in June 2004. I gave birth by caesarean section and that is when my problems started. The baby died. I went to the hospital in Bururi but they could not help me. They told me only Roi Khaled Hospital could help me. I had so many health problems for a year, but I didn't have the money to get better. Finally I decided to come here, even without money. I have two other children and it was too hard because I was so sick all the time. Since I have been here, I have had two operations and I am not totally healed now, but it is better.... Now, I would prefer to go back home to finish healing but I cannot leave here.112
Gabriel N., from Cibitoke, spent five months in the hospital following an automobile accident. He was fortunate to find a benefactor who paid his bill and he went home, even though he was not yet completely healed. He said, "The bill was too high for me to ever be able to pay myself."113 Three months later, Gabriel N. fractured his leg and severely injured his mouth in a motorcycle accident. He stayed at home, hoping to heal on his own, but went back to the hospital after his wounds became infected. He had surgery to repair the fractured leg. "After that surgery, I told the doctor not to treat me too much," he said, "because I knew I wouldn't be able to pay for the costs of the treatment." At that time his bill amounted to about U.S.$275. Doctors suggested surgery to repair the damage to his mouth, where several of his front teeth had been crushed into his lip and gums, making talking and eating difficult. Gabriel N. refused, reluctant to complicate his situation further. He remained detained, however, because he could not pay the $275.114
Delaying treatment can lead to further complications and the need for more extensive – and expensive – care. This ultimately increases the likelihood of detention once care is sought. For others, care is simply not sought at all, leading potentially to disability and even death.
VII. The Government Response
The government has an immediate duty to end the detention of poor patients for non-payment of their medical bills, and a longer-range responsibility to progressively realize the right to health of its citizens. Senior government officials and hospital staff alike often deny or minimize the problem of hospital detentions. The chef de cabinet in the Ministry of Health told us,
In my opinion, this is not detention or imprisonment. It is a long waiting period. If people cannot pay at all, they are allowed to go. They might overstay two to three days or a week.115
The director of Prince Louis Rwagasore Clinic said,
We have a small hospital so we let people [who cannot pay] leave because we realize they cannot pay, or because they find a benefactor. As soon as people have recovered, they are released. We just keep the bills. One speaks about prisoners but in reality there are no prisoners. They themselves say tomorrow, the day after tomorrow a person will come and pay for me.116
The director of Roi Khaled Hospital declared that "this is not a prison," and said that people who cannot pay their bills are released.117 Several hospital managers questioned the use of the word "detention."118
The reality was different, as shown above. In nine of the eleven hospitals we visited, patients were detained, and many of them for far longer than one week. While denying or minimizing the problem, government and hospital officials contradicted themselves by attempting to justify hospital detentions. According to the chef de cabinet in the Ministry of Health:
Hospitals managers have to ensure financial stability. If the directors don't pay attention, they have to shut down the hospital.119
The chef de cabinet in the Ministry of National Solidarity, as well as several hospital managers, echoed this argument, pointing out that hospitals would have to close if they lacked the funds to operate. Others suggested the alternative was to refuse treatment.120 Government and hospital officials alike presented the issue as deplorable but refused to take responsibility for it.
In December 2005, the Ministry of National Solidarity – apparently at the initiative of the president – ordered the release of patients and announced it would pay for their bills. The move was widely reported in the press, and one formerly detained patient we spoke to expressed her gratitude to the president for this initiative. The minister's chef de cabinet reportedly told hospitals that they should release their detainees and send the bills to her Ministry. But when asked by the press whether detentions in hospitals would now end, she replied evasively,
There is no reason to believe that the problem of insolvability will be resolved if the majority of the population continues to live in conditions of extreme poverty. To eradicate this phenomenon completely, one needs a series of projects that allow people to pay for their medical treatment.121
To the dismay of hospital officials, the government did not reimburse the bills as promised. By May 2006, the government owed the four major hospitals over U.S.$50,000.122 According to the chef de cabinet, the responsibility for the non-payment lay not with her Ministry, but with the Crédit de Relance Economique, a World Bank-financed fund for reconstruction activities.123
Ad-hoc measures such as the December 2005 "charitable" release of detainees in hospitals may bring the government good publicity but do nothing to solve the real problem. Shortly after Christmas 2005, hospitals were again filling up with insolvent patients in detention.
VIII. Government Measures Aimed to Improve Access to Health Care
The failure of health insurance
The Burundian health system uses mechanisms that are supposed to increase access to health care for the poor. If functioning effectively, these mechanisms could allow some of the poor to pay their medical expenses and avoid hospital detention. An illness insurance card (carte d'assurance maladie, CAM) costs U.S.$0.50 per year and covers 80 percent of some, but not all medical, costs.124 The CAM is a voluntary, community-based prepayment scheme that is open to all. It is particularly meant for the poor, and complements a compulsory insurance scheme for civil servants.125
In practice, health insurance rarely, if ever, works well enough to keep poor people from detention in hospitals. Recognized as ineffective, the card is little used in most of the country and has been abolished in five of seventeen provinces. The 2005 National Plan for Health Development says that "the population does not have confidence in the illness insurance card (CAM) any more... This card is in the process of disappearing in most parts of the country."126 Only 1 percent of patients surveyed by the MSF study mentioned above had the insurance card.127
In our own interviews, we spoke with over 20 hospital detainees who had the insurance card but still ended up in hospital detention. Many patients did not have insurance when they entered the hospital, but obtained it with the help of their family on the day they were hospitalized, or later. Hospitals sometimes rejected the illness insurance card when it was bought at this late date. Claudine N., whose newborn baby needed lifesaving surgery, told us,
I obtained the insurance card after I came to hospital. My husband got it for me at the commune, and it cost 500 FBU [$0.50]. But they did not accept it at the hospital. You are supposed to get it before you come.128
Large hospitals like Roi Khaled Hospital and Prince Régent Hospital also excluded medical equipment and supplies from the costs covered by insurance. Dorothée H., mentioned above, needed a hip replacement but was told that her insurance did not cover the $400 cost.129 Other hospitals, like Prince Louis Rwagasore Clinic, do not accept the insurance at all.130
Some provincial hospitals, like those at Gitega and Ngozi,131 accepted the insurance and Gitega Hospital even promoted it. Yet even in these hospitals patients were detained if they could not pay the remaining 20 percent of the costs. Such was the case of two women detained at Gitega Hospital after having had surgery for birth complications.132
The failure of the exemption system for the poor
In Burundi, people with no financial means at their disposal, defined as "indigent" by their local administrators, may receive an indigence card (carte d'indigence) that makes them exempt from paying health care costs, as well as from educational and other fees. Since 2003, those who have been displaced by the war may also qualify for a voucher that exempts them from health care costs.
However, criteria for receiving both the indigence card and the vouchers are not officially defined, leaving the process lacking in transparency and open to arbitrary decisions. According to MSF, "the exemption system has become a sectoral and clientelistic practice."133 These faults in the procedure make it even more likely that the systems meant to provide relief to the poor actually deliver little but token help to a few.
The indigence card
When poor people receive the indigence card, the commune of residence of such persons is then required to pay their medical bills. The government points to the system as proof of its will to assist the needy, but the system rarely provides exemptions for the poor, and simply hides lack of effective government action. A local administrator in Bujumbura-rural province explained to us,
We as communal administrators are charged with handing out the indigence card. We know who is vulnerable: orphans, very old people, people without land, people who live from begging, sometimes people without children to support them. If someone like this gets sick, neighbors take them to the commune. For small things, we can take them to the health center run by GVC and ECHO [Gruppo Voluntariato Civile and the European Commission's Humanitarian Aid Office, both humanitarian agencies]. But for big things, like an operation, we cannot help them now. Even if I gave them the necessary document, it does not have any meaning. The commune is responsible for paying these bills and we do not have a budget for that.134
In its recent National Plan for Health Development (Plan national de développement sanitaire), the government itself admits that most communes do not provide indigence cards any more.135
Most hospital detainees we interviewed did not have an indigence card and had not even heard about it. The study by Save the Children, mentioned above, found that only about 10 percent of all people surveyed knew there was a system to exempt the poor from health care costs, and only 4 percent of the poorest households interviewed knew about it.136 Our research found that those who did have the indigence card, or tried to get it, encountered difficulties. As noted above, Christian B., an orphan suffering from a chronic skin disease, was told by his local administrator that the card was no longer in use.137
Other patients who had the card had it rejected by the hospital. For example, Désirée N., a woman from Bubanza province who came to Roi Khaled Hospital because she was pregnant and had a tumour, gave birth prematurely and the child needed an incubator. As she was destitute, she was detained – four weeks at the time of the interview – and did not get the tumour treated. She said that she had an indigence card but that the hospital had rejected it.138 The director of Roi Khaled hospital told us that "the hospital does not accept the indigence card because the state does not reimburse its expenses." He added that displaced people and returnees could get vouchers until the end of 2005, but not any more.139 A nurse at the same hospital confirmed that staff had been instructed not to accept the indigence card.140 This is also the case for other hospitals.141
The voucher for displaced people
In recent years displaced people and returnees with an indigence card were eligible for vouchers at the National Commission for the Reintegration of the Displaced (Commission Nationale pour la Réintegration des Sinistrés,CNRS). 142 The CNRS was an agency established under the Arusha Accords to aid "all displaced, regrouped and dispersed persons and returnees."143 Funded by the government and donors, it functioned from mid-2003 to December 2005.144
Local administrators sometimes handed out indigence cards when they were confident that the CNRS would reimburse them. However, this was not often the case, as a local administrator criticized:
For a while, the CNRS was able to pay some bills. But you had to find someone who could "do gymnastics" to ever get any money there. If I thought a family had someone who could manage to get help from CNRS, I would give them the indigence card and sometimes they could get some money, but often not.145
Other officials familiar with the process echoed his concern about the "management and money problems" at the agency.146
The procedure for obtaining vouchers was such a burdensome and complex process that few potential recipients pursued it to the end.147 If they did obtain a voucher, it could be used at only three hospitals, all in Bujumbura. For a patient to be permitted to leave the hospital at the conclusion of treatment, the hospitals would have to agree to accept the voucher and then transmit the bills to the office of the CNRS to be reimbursed.148 Poorly designed, the system was also badly managed and some funds, according to officials involved, were misused.149
The CNRS, a structure of the transitional government, ended when the newly elected government took power, but a government body called PARESI has been created to succeed it, and the Fund for Victims continues to exist, reassigned to the Ministry of National Solidarity, Human Rights, and Gender. According to the chef de cabinet of the Ministry, the fund held 500 million FBU in 2006 ($500,000).150 The criteria for receiving assistance are unclear, in particular whether only displaced people and returnees are eligible for help or whether other needy persons may also apply. According to an official charged with distributing vouchers, displaced and repatriated people are often better treated and have better access to free medical care than other indigent people. When there is a lot of media attention on a certain case, for example if a woman has triplets, the Ministry will help her, but in general other needy people will be turned away.151

A patient detained at Prince Régent Charles Hospital. © 2006 Jehad Nga
Alternatives to hospital detention
Some hospitals have found ways other than detention to assure payment of bills, though these alternatives can create other problems for patients. Hospitals in Muyinga (northeastern Burundi) and Matana (southern Burundi) keep the identity cards of patients who are unable pay.152 Such former patients then feel pressure to pay because security forces frequently ask to see identity cards, and anyone without one may be considered suspicious and even taken as a possible supporter of the FNL rebels. When an indebted patient has a bicycle, the hospital in Muyinga also retains this essential means of transport in order to increase pressure to discharge the debt.153
In some health centers staff get former patients to work off their debt by cultivating fields belonging to the health center.154 Staff of the Prince Louis Rwagasore Clinic allow patients with stable employment to leave once they agree to have the money owed deducted from their salaries and paid directly to the hospital by their employers.155 This strategy is useful only in urban settings where patients are salaried workers.
Some facilities supported by international NGOs operate a different model of health financing: the patients pay a percentage of the costs, as in Makamba province where they pay 50 percent of the medicine plus cost of treatment, or a flat fee, as in Karuzi, Cankuzo, Bujumbura-rural and Ruyigi provinces, where patients pay an all-inclusive charge ranging from 50 to 500 FBU ($0.05 to $0.50).156 As a result, detention of patients is unusual in these hospitals. At Buhiga Hospital in Karuzi, where patients pay 300 FBU [$0.30] for out-patient treatment and 500 FBU [$0.50] for hospitalization, there were no detainees at the time of a visit by some of our research team to the hospital in March 2006. According to the financial and administrative director, there were patients who could not pay the flat fee, but they are treated at Karuzi nevertheless.157 In Bururi province, the Dutch agency Cordaid started a new scheme for indigent patients in January 2006, sponsoring medicine and consultations, and soon after there were no hospital detainees there.158
Free care for women giving birth and small children: The May 1 presidential directive
On Labor Day, May 1, 2006, President Nkurunziza declared that all maternal health care and treatment for children under five years old would henceforth be free of charge.He also announced pay rises for public service employees, and the creation of an anti-corruption brigade.159
The ruling CNDD-FDD portrays itself as a popular movement addressing the needs of the poor. Shortly after coming to power, the new government abolished primary school fees and introduced free and compulsory primary education.160 The government health plan of December 2005 focused on improving maternal and infant health through improved obstetric care at health centers and hospitals; the creation of a fund for caesarean deliveries and complicated births; improved antenatal care; subsidies for medicine for the poor; and health care for children under five years old.161
The introduction of free health care for pregnant women, mothers and small children is part of the government's self-proclaimed effort to reach out to the poor.162 Perhaps more importantly, it also aims to show donors the government's willingness and ability to use funds well. It constitutes concrete progress towards two Millennium Development Goals – reducing child and maternal mortality.Under the Heavily Indebted Poor Countries Initiative, a country's debt can be reduced if certain economic and social conditions are fulfilled. Burundi is currently getting debt relief on an interim basis, and it is striving to qualify for permanent debt relief. According to one hospital manager, "The government has received debt relief funds, and now they need to be used."163
Some observers have also noted that increased pressure regarding the detention of hospital patients might have played into the decision.164 Prior to the announcement of the reform, the Burundian government and the World Bank were discussing how to best use the $10 million gained from debt relief, and the release of detained patients was one of the issues that arose.165
While the directive on free maternal and child health appears to be a very good idea, in practice it has caused serious problems.
An increased burden on the health system
During the first days of May 2006, thousands of pregnant women and parents of sick children made their way to the nearest hospital to benefit from the reform. According to a manager at Prince Louis Rwagasore Clinic in Bujumbura:
Our hospital is overwhelmed with patients, and we have insufficient capacity.... We have four tables for delivery and sometimes ten women arrive at the same moment, so you can imagine the problem. We have sometimes run out of sterilization equipment and sent women elsewhere.166
At Bururi Hospital, the number of patients in the maternity ward rose from a daily average of 14 a day to at least 40. At Kayanza Hospital, where there was already an acute lack of medical staff, the single doctor able to perform caesarean deliveries was overwhelmed.167 Rumonge Hospital ran out of medicine or supplies only days after the presidential directive.168 Roi Khaled Hospital ran out of essential materials and had to ask suppliers to fill their orders without immediate payment.169 As hospitals were overstretched, some patients were denied treatment. A woman with a miscarriage died at Roi Khaled Hospital, after medical staff in this and other locations reportedly turned her away.170
Many ordinary Burundians have expressed enthusiasm for the initiative. However patients have also criticized that hospitals do not always pay for the medicine for beneficiaries.171 The reform foresees free medicine only for those future mothers and small children who are hospitalized; outpatients – those who do not stay at the hospital – have to pay for their medicine themselves.172
One of the main problems of the May 1 presidential directive was the lack of preparation for the reform. Hospitals learned of the change on the radio, which meant that they had no chance to prepare in advance for the influx of new patients.173 Even the chef de cabinet in the Ministry of Health recognized this problem: "When the President declared free health care [for women giving birth and children under five], the hospitals were not ready in terms of medicine, equipment, staff numbers and housing capacity. Now we are dealing with these problems."174 Many health administrators and hospital managers also criticized the way the reform was launched so suddenly, a sentiment shared by representatives of donor nations as well.175
According to the World Health Organization, the government and donors decided that about $3 million of the $10 million to be made available in the context of debt relief were to go to essential medicines and health care for children and costs of childbirth. Some of these funds could be used to pay for maternal and child health care176 and other funds might have an indirect impact on access to health care. But funds would still be insufficient to pay for the new initiative, which were not covered in the regular budget.177 The Ministry of Health may ask donors for more support but first, said one official, "we have to negotiate with the government itself to show the gap in funding."178 By early August 2006, the Ministry had managed to get some additional government funds, but these "are not sufficient at all" and the government continued to seek further funds.179 In late June hospitals began sending their bills for the costs of the new program to the government, anxious to see whether they would be reimbursed as promised. Bills at Prince Louis Rwagasore Clinic and Roi Khaled Hospital were roughly $20,000 each.180 By early August they had not been reimbursed.181
The introduction of free maternal and child health care constitutes an important step towards the progressive realization of the right to health, in particular achieving the reduction of the stillbirth rate and infant mortality.182 But the policy will fail if the government does not urgently take the measures to ensure the program's sustainability and increase staff, equipment and medicine throughout the country. Furthermore, the government must embed the new, badly prepared change in the context of a larger health policy.
Impact on hospital detentions
The May 1 reform meant that women giving birth and children under five years old are no longer detained in hospitals, thus significantly reducing (by about one third) the number of persons suffering from this abuse. In June 2006, for example, there were no women with birth complications or children under five detained at Roi Khaled and Prince Régent Charles Hospitals.
The presidential directive also spurred other initiatives. The Ministry of National Solidarity, Human Rights and Gender paid about $13,000 to free women with birth complications and children under five who had been detained at Roi Khaled Hospital between January and May 2006.183
Yet the majority of detainees have not benefited from the reform as it does not apply to them. Women with problems unrelated to childbirth, children over the age of five, and men continue to be detained. In late June 2006, 36 patients were held at Roi Khaled Hospital and 41 at Prince Régent Charles Hospital.184 A staff member at Prince Louis Rwagasore Clinic also confirmed that the practice continued at his hospital.185
Among those held at Roi Khaled Hospital was Jerôme N., a 17-year-old boy who suffered a serious leg infection, and who could not walk. He was detained for almost one month at the time of the interview, and told us,
My mother left here and sold a piece of our land to help pay for the medicine. We had to pay for the medicine up-front before the surgery could even be done, so she sold the land for 300,000 FBU [$300] to pay for the medicine. By the end of March, I felt much better. I have now been completely healed for a month but I cannot leave the hospital because I have the bill of more than 700,000 FBU [$700] for the operation. The doctor came and told me that I am healed but that I cannot leave because I cannot pay. Yesterday they told me to leave my bed so a paying patient could have it, so I slept on the floor on a mat that someone lent me. I tried to escape once but the guards at the gate said that I couldn't leave and I didn't have an authorization to leave.186
Among those held at Prince Régent Charles Hospital was Augustin M., a 26-year old man from Muyinga province who had a car accident. He told a Human Rights Watch researcher,
Two weeks ago, the doctors told me that I was healed, but I could not pay the bill, so I had to stay here. I have no money and no land and no work, and I need another operation to take the metal rod out of my leg. The nurse told me that they might not take out the metal rod if I cannot pay for the first surgery.... I feel like a prisoner here because I cannot leave. I am afraid I will have the metal rod in my leg forever....The [government] declaration is good but I think that other people should be covered, like those who have no father. He died when I was young and my mother has no money.187
Not surprisingly these and other victims detained expressed hope that the government would extend the reform to their cases as well.188

Twenty-year-old Albert H. was hurt in a car accident when he went to check on his family's farm, which they had fled a year earlier. He sustained injuries to his eye and left arm. When he could not pay the bill, he was detained at Prince Régent Charles Hospital in Bujumbura. © 2006 Jehad Nga
Further government plans for health reform
In its National Plan for Health Development, the Ministry of Health says it intends to raise the health budget to about 15 percent of the total annual budget (from about 2.7 percent in 2005189), in line with a commitment made by African countries in 2001.190
The plan also acknowledges that the current medical insurance system is not working properly and proposes abolishing it and replacing it with a system of mutuelles. These are voluntary community-based health insurance schemes that function somewhat like a cooperative. The Burundian government proposes to promote these for the population that is active in the informal urban or rural sectors of the economy – that is, large parts of the population. While community-based health insurance is traditionally created and funded totally through a local community, the Burundian government gives the state a more important role, as it is planning to subsidize them.191 Studies have shown that low enrollment is a frequent problem of community-based health insurance. Should the government go ahead with its plan to create mutuelles, it will need to develop a strategy for how to address this problem and make mutuelles viable for the poor who are active in the rural or urban informal economy.
In its national health plan, the government makes a somewhat artificial distinction between those who work in the informal sector and those who are poor. It suggests that there might be difficulties in extending community-based health insurance schemes to the poor and proposes state subsidies to "protect the most vulnerable groups such as pregnant women (all), children under five years of age and indigents."192 While the government has, as already discussed, taken steps to improve access to health care for pregnant women and small children, it has not done so for indigents. The Ministry of Health has attempted to create a fund for poor patients but this was rejected during the budget debate in December 2005.193 The plan remains vague and does not mention the problem of hospital detentions. In August 2006 the Burundian government was working on the final touches of the country's Poverty Reduction Strategy Paper (PRSP), the draft of which repeats the same health policy priorities but does not provide any additional detail. It also does not mention hospital detentions.194
IX. Government Failure to Address Other Structural Problems of the Health System
Starving the hospitals: The downside of hospital autonomy
When hospitals were made autonomous beginning in 1988, they had to assume responsibility for financing most of their activities. If they fail to recover past costs, they must cut future expenses; in many cases this includes staff salaries.
The state owes hospitals large sums of money under the medical insurance system. According to management staff at the Prince Régent Charles Hospital, insurance bills from 2004 and 2005 are still outstanding.195 The Ministry of Finance, responsible for paying bills, pays them with less and less regularity as the year goes on and, according to one hospital official, "by June the payments stop."196 The overall budget for medical insurance was 180 million FBU (U.S.$180,000) in 2005 and 300 million FBU ($300,000) in 2006.197
The government pays a subsidy to public hospitals, but this support covers only a fraction of their costs. Prince Louis Rwagasore Clinic, for example, receives about 10 percent of its annual budget from the state198 and Prince Régent Charles Hospital about 30 percent.199 Salaries of health personnel are very low, in part because state assistance to hospitals is so limited. The starting salary of a general practitioner in 2004 was 62,980 FBU ($62) per month.200
Lack of transparency in health sector finance
The Burundian health sector is plagued not just by lack of funds but by lack of clear guidelines, as well as fraud and corruption, in how they are used.
Hospital staff are uncertain when and how much of their institution's expenses will be reimbursed by the state because the medical insurance and indigence card systems do not work properly. Poor patients are unsure what costs they will have to pay.
Hospital staff have themselves been involved in financial mismanagement and corruption. In October 2005, officials at the CNRS found Roi Khaled staff submitting false vouchers and fabricating and selling documents attesting to poverty or returnee status. The supposed organizer of the fraud, an employee of the CNRS based in the hospital, was suspended.201 According to an official in the Ministry of National Solidarity, Human Rights and Gender, cheating and fraud remain a problem at the Fund for Victims.202International agencies that pay hospital bills for some of their beneficiaries have complained of cases of false or inflated bills prepared by hospital staff.203
On February 24, 2006, the finance minister acknowledged in a radio broadcast that one billion FBU ($1 million) had come through the treasury, supposedly for the purchase of medicine, but that he could not account for its use.204 Shortly after, health officials deplored the disappearances of medicine from health centers and expressed concern that there might be "deliberate speculating by health center managers" in the sale of medicine.205
Among past indications of corruption in the health sector was the 2001 murder of Kassi Manlan, head of the World Health Organization in Burundi, reportedly killed because he had uncovered embezzlement by important Burundian officials of money meant to buy medicines.206
Following the president's announcement of anti-corruption measures, parliament voted in July 2006 for the creation of an Anti-Corruption Brigade with police powers, despite worries about the constitutionality of the body.207
X. Keeping the System Alive: The Dilemma of Being a Benefactor
As shown above benefactors in the form of private individuals, churches or organizations sometimes paid off the debts of patients so they could go home.
The number of benefactors has risen in the last few years, according to statistics and observations by hospital staff. At Prince Régent Charles Hospital, the figure has more than quadrupled between 2004 and 2005, as mentioned above. Like similar interventions by the government, freeing individuals renders them immediate assistance but provides no permanent solution to the problem of hospital shortfalls. Such acts of generosity may have even encouraged the practice by in effect rewarding hospitals that detained people.
In at least one facility, the Roi Khaled hospital, the presidential directive on maternal and child health has led to a decline in the number of benefactors, presumably because they believe private charity is no longer so necessary.208 It is too soon to say whether the recent decrease in one institution will continue and will be replicated in other hospitals.208 Human Rights Watch telephone interview with financial and administative director, Roi Khaled Hospital, June 20, 2006.
XI. The Role of the International Community in the Health Sector
Donor aid
In 2000, the international community set itself ambitious development targets, the Millennium Development Goals, including major progress on combating child and maternal mortality, HIV/AIDS, and malaria. The Millennium Project report on goals four and five (reducing child and maternal mortality) recommends that "bilateral donors and international financial institutions should substantially increase aid" to the health sector. It also recommends that user fees for basic health services be abolished.209 Donors committed themselves, at the 2002 Monterrey Conference210 and subsequently, to funding the initiative; in particular rich countries pledged to devote 0.7 percent of their gross national product to official development assistance. However, to date, only a few countries have done so,211 and attaining the health-related Millennium Development Goals remains a distant prospect.
In Burundi, aid flows have been heavily affected by the political crisis and armed conflict. Following Pierre Buyoya's 1996 military coup, countries in Central Africa imposed economic sanctions on Burundi, and international aid was reduced by two-thirds.212 With the Arusha Peace Agreement at least partly implemented and the political transition moving ahead, many donors recently renewed aid. In late February 2006, the government held a donor conference to request funds for improved health care, aid to drought-stricken regions, and other programs needed to help rehabilitate the damaged country.213 In the coming period, donors are expected to shift their aid from humanitarian assistance to development aid. As already noted above, in August 2006 the Burundian government was working on the final touches of the country's Poverty Reduction Strategy Paper. The PRSP offers a long-term development plan and forms the basis for decisions about future donor funding, debt relief and loans from the international financial institutions.214 The completed PRSP will be presented to the World Bank and made public.
At present, the European Commission (EC) is the most significant multilateral donor, currently providing about €72 million (U.S.$92 million) through various channels including the European Development Fund (EDF) and the European Commission Humanitarian Office (ECHO). It provides about €31 million ($39 million) in budgetary support.215 Belgium and France are the two largest bilateral donors: they support the government budget and fund particular projects in the areas of rule of law, health and education. The United States is providing approximately $30 million per year in non-food humanitarian and development assistance.216 Germany is supporting the government with about €44.5 million ($57 million), primarily in the area of improving water supply.217 The UK government provides about £10m ($19 million) to Burundi for 2006-07, of which about one-third is destined for the health sector.218 In addition, nongovernmental agencies such as Cordaid, MSF and ActionAid fund particular areas of the health sector.
Despite the commitments of international donors to assisting Burundi in the area of health, donors have not pressed effectively for an end to the detention of patients, and improved access to health care for the poor.
Debt relief
Under the Heavily Indebted Poor Countries Initiative, Burundi has qualified for the initial phase of interim debt relief, subject to meeting certain conditions. During this period, the World Bank and the International Monetary Fund have imposed a limitation on the use of the funds and determined that they must go towards education, health and agriculture.219 As a result, the government has almost tripled the health budget from about $5 million to about $15 million. Burundi is currently completing the economic measures essential to finalizing the debt relief agreement in 2006. Once Burundi has permanent status, the government is in theory free to set its own spending priorities and is not required to fund key social sectors.220
Nonetheless, the government has pledged to spend the debt relief funds on health, education, infrastructure, agriculture, the settlement and reintegration of victims of civil strife, and judicial reform. It has also promised to set up an independent oversight committee composed of international and national representatives, to monitor expenditures.221
XII. Human Rights Standards
The detention of patients who are unable to pay their medical bills at public hospitals in Burundi raises a number of concerns under international human rights law. This includes the right not to be arbitrarily detained, detained as a debtor or mistreated in detention as protected in the International Covenant on Civil and Political Rights (ICCPR). The impact of the policy on individuals seeking health care implicates the state's progressive realization of the right to the highest attainable standard of health under the International Covenant on Economic, Social and Cultural Rights (ICESCR) and other human rights instruments. Burundi became a party to both covenants in 1990.
Detention
The detention of debtors – such as persons who are unable to settle their hospital bill – is unlawful under international human rights law. Article 9 of the ICCPR provides that everyone has the right to liberty and security of person and "[n]o one shall be subjected to arbitrary arrest or detention." Detention is considered arbitrary if it is illegal or if manifestly disproportionate, unjust, discriminatory or unpredictable.222
More specifically, article 11 of the ICCPR states: "No one shall be imprisoned merely on the ground of inability to fulfill a contractual obligation." This provision prohibits the deprivation of personal liberty for failure to pay a debt either by a creditor or by the state. States have an obligation to enact laws and other measures to prevent the state and private creditors from limiting the personal liberty of their debtors who cannot fulfill their contracts.223
The ICCPR lays out the right to humane treatment in detention. Article 10 states that all persons deprived of their liberty shall be treated with humanity and with respect for the inherent dignity of the human person. In its General Comment, the Human Rights Committee, the international body of experts that monitors compliance with the ICCPR, has made clear that this article applies to:
[A]ny one deprived of liberty under the laws and authority of the State who is held in prisons, hospitals - particularly psychiatric hospitals - detention camps or correctional institutions or elsewhere. States parties should ensure that the principle stipulated therein is observed in all institutions and establishments within their jurisdiction where persons are being held.224
Patients who are held in state hospitals come within the protection of article 10.
Health
Health is a fundamental human right enshrined in numerous international human rights instruments, including the Universal Declaration of Human Rights, the ICESCR, the African Charter for Human and People's Rights, the Convention on the Rights of the Child, and the Convention on the Elimination of All Forms of Discrimination against Women (CEDAW). The ICESCR specifies that everyone has a right "to the enjoyment of the highest attainable standard of physical and mental health."225
Because states have different levels of resources, international law does not mandate the kind of health care to be provided, beyond certain minimum standards. The right to health is considered a right of "progressive realization." By becoming party to the international agreements, a state agrees "to take steps... to the maximum of its available resources" to achieve the full realization of the right to health. States are obliged to create conditions that would assure access to all medical service and medical attention in the event of sickness.226
The Committee on Economic, Social and Cultural Rights provides examples of what constitutes a failure of a government to fulfill its obligations with respect to the right to health. The examples include failing to adopt or implement a national health policy designed to ensure the right to health for everyone; insufficient expenditure or misallocation of public resources which results in the non-enjoyment of the right to health by individuals or groups, particularly the vulnerable or marginalized, and the failure to reduce infant and maternal mortality rates.227
International law describes essential elements of the right to health (availability, accessibility, acceptability and quality), as well as minimum "core obligations" of governments. The basic elements of this right and the minimum core obligations are described in detail in General Comment No. 14 of the Committee on Economic, Social and Cultural Rights. That General Comment emphasizes the minimum core obligations of a government in terms of health care, which includes, for example, "the right of access to health facilities, goods and services on a non-discriminatory basis, especially for vulnerable or marginalized groups" and that governments must "ensure equitable distribution of all health facilities, goods, and services."228 With regard to economic access, the Committee states:
Health facilities, goods and services must be affordable for all. Payment for health-care services, as well as services related to the underlying determinants of health, has to be based on the principle of equity, ensuring that these services, whether privately or publicly provided, are affordable for all, including socially disadvantaged groups. Equity demands that poorer households should not be disproportionately burdened with health expenses as compared to richer households.229
In this perspective, the recent decision by the Burundian government to make maternal and child health care free of charge constitutes an important advance in progressively realizing the right to health.
Under international law on the right to health, priority is given to children and women. The ICESCR stipulates that efforts must focus on child and maternal health, that is by taking measures to reduce the stillbirth rate and infant mortality and to provide for the healthy development of the child.230 The Committee on Economic, Social and Cultural Rights states that ensuring "reproductive, maternal (pre-natal as well as post-natal) and child health care" is of comparable priority to the core obligations. Lowering of maternal mortality is defined as a "major goal" for governments.
Building upon the provisions of the ICESCR, the Convention on the Rights of the Child has specified the particular rights of children with regards to health, and states that governments must act in the areas of child health and pre-and post-natal health care, in particular primary health care.231 Similarly, the CEDAW defines the right of women to access health care without discrimination and to get "appropriate services in connection with pregnancy, confinement and the post-natal period, granting free services where necessary, as well as adequate nutrition during pregnancy and lactation."232
XIII. Acknowledgements
This report was written by Juliane Kippenberg, NGO liaison in the Africa division of Human Rights Watch. It is based on field research conducted by Juliane Kippenberg, Maria Burnett, Burundi researcher at Human Rights Watch, Jean-Baptiste Sahokwasama, legal representative of APRODH, Ladislas Gahungu, assistant psychologist at APRODH and APRODH observers based in the provinces of Burundi. Béatrice Nicitegetse provided research assistance and translated the interviews.
The report was edited by Maria Burnett. It was reviewed at Human Rights Watch by Alison Des Forges, senior advisor on the Great Lakes; Joseph Amon, director of the HIV/AIDS and Human Rights division; Tony Tate, researcher in the Children's Rights division; Janet Walsh, acting director of the Women's Rights division; James Ross, senior legal advisor; and Ian Gorvin, consultant to the Program Office. At APRODH, it was reviewed by Jean-Baptiste Sahokwasama and Ladislas Gahungu.
Production assistance was provided by Lizzie Parsons, associate in the Africa division, Veronica Matushaj, photo editor, Andrea Holley, productions director, Juliette Le Doré, press associate, Ella Moran, creative associate, and Fitzroy Hepkins. Isabelle Thomas translated the report into French.
Jehad Nga, photojournalist, took all the photographs in this report, and generously donated them to Human Rights Watch.
We would like to thank all patients who agreed to speak to us while in hospital. We would also like to thank directors, financial directors, doctors, nurses, social workers and other staff at Roi Khaled Hospital, Prince Régent Charles Hospital, Prince Louis Rwagasore Clinic, Ngozi Hospital, Gitega Hospital, Muramvya Hospital, Karuzi Hospital, Muyinga Hospital, Bururi Hospital, Matana Hospital and Rumonge Hospital for providing valuable insights and facilitating our research.
1 There are 35 hospitals in Burundi.
2 Human Rights Watch, "Burundi: Missteps at a Crucial Moment", A Human Rights Watch Report, November 4, 2005, http://hrw.org/backgrounder/africa/burundi1105/; Human Rights Watch "Warning Signs: Continuing Abuses in Burundi", A Human Rights Watch Report, February 27, 2006, http://hrw.org/reports/2006/burundi0206/; Human Rights Watch, "A Long Way From Home: FNL Child Soldiers in Burundi", A Human Rights Watch Briefing Paper, 16 June 2006, http://hrw.org/backgrounder/africa/burundi0606/.
3 "Burundi: Rebels attack civilians as ceasefire talks continue", IRIN, July 19, 2006, http://www.reliefweb.int/rw/RWB.NSF/db900SID/EVOD-6RUKB2?OpenDocument&rc=1&cc=bdi (accessed July 21, 2006).
4 United Nations Development Programme (UNDP), Human Development Report 2005 (New York: United Nations Development Programme, 2005), http://hdr.undp.org/reports/global/2005/pdf/HDR05_HDI.pdf (accessed May 4, 2006).
5 United Nations Childrens' Fund (UNICEF), Burundi Statistics, http://www.unicef.org/infobycountry/burundi_statistics.html (accessed May 5, 2006).
6 World Health Organization (WHO), "Burundi, Health Sector Needs Assessment," (undated), http://www.who.int/hac/donorinfo/cap/burundi.pdf (accessed July 21, 2006).
7 Infants are children under one. Figures from UNICEF background information on Burundi, at http://www.unicef.org/infobycountry/burundi_statistics.html (accessed July 27, 2006). Analysis from WHO, "Burundi, Health Sector Needs Assessment."
8 T. Niyongabo, A. Ndayiragije, B. Larouze and P. Aubry, "Burundi: Impact de dix années de guerre civile sur les endémo-épidémies," Médicine Tropicale, vol. 65, 4 (2005), pp. 305-311.
9 Human Rights Watch/APRODH interview with director and other managers, Prince Louis Rwagasore Clinic, Bujumbura, February 14, 2006.
10 Mit Philips, Gorik Ooms, Sally Hargreaves and Andrew Durrant, "Burundi; A population deprived of basic health care," The British Journal of General Practice (August 2004), pp. 634-635; Save the Children, "The Cost of Coping with Illness," Briefing, November 2005, p. 1.
11 See section VIII.3 on Alternatives to hospital detention.
12 République du Burundi, Ministère de la Santé, "Plan national de développement sanitaire 2006-2010," Bujumbura, December 13, 2005, p. 19; Human Rights Watch/APRODH interview with Dr. Julien Kamyo, chef de cabinet, Ministry of Health, Bujumbura, February 13, 2006.
13 Médecins Sans Frontières (MSF), "Access to health care in Burundi. Results of three epidemiological surveys," April 2004; Philips et al., "Burundi; A population deprived of basic health care."
14 République du Burundi, Ministère de la Santé, "Plan national de développement sanitaire 2006-2010."
15 World Bank, "Cost Sharing: Towards Sustainable Health Care in Sub-Saharan Africa," Findings – Africa Region, No. 63 (May 1996), http://www.worldbank.org/afr/findings/english/find63.htm (accessed August 8, 2006).
16 Equity is a term used frequently in development to describe the principle of fairness in accessing resources. For a fuller definition, see Maureen Johnson, "The Challenge of Achieving Health Equity in Africa," Science in Africa, June 2004, http://www.scienceinafrica.co.za/2004/june/equity.htm (accessed May 5, 2006).
17 Timothy Poletti, "Cost-recovery in the health sector: an inappropriate policy in complex emergencies," Humanitarian Exchange, No. 26 (March 2004). For a wider assessment of cost recovery models, see Sanjay Reddy and Jan Vandemoortele, User Financing of Basic Social Services. A Review of theoretical arguments and empirical evidence (UNICEF, 1996), http://www.unicef.org/evaldatabase/files/Global_1996_User_Financing_part_1.pdf [and part_2.pdf and part_3.pdf] (accessed August 9, 2006).
18 V. Ridde and J.-E. Girard, "Twelve years after the Bamako Initiative: established facts and political implications for greater equity in access to health services for indigent Africans," Santé publique, vol. 15, no. 1 (2004), pp. 37-51; Reddy and Vandemoortele, User Financing, pp. 50-53.
19 MSF, "Access to health care in Burundi"; Philips et al., "Burundi; A population deprived of basic health care."
20 République du Burundi, Ministère de la Santé, "Plan national de développement sanitaire 2006-2010,"p. 21. This was confirmed by MSF/Belgium in Burundi.
21 Poletti, "Cost-recovery in the health sector"; Mark Pearson, "The Case for Abolition of User Fees for Primary Health Services," DFID Health Systems Resource Centre issues paper, September 2004, http://www.eldis.org/fulltext/pearson2004.pdf (accessed May 19, 2006).
22 U.S.$1 is about 1000 Francs Burundais (FBU), http://finance.yahoo.com/currency (accessed August 24, 2006)
23 Ridde and Girard, "Twelve years after the Bamako Initiative"; Masuma Mamdani and Maggie Bangser, "Poor People's Experiences of Health Services in Tanzania: A Literature Review," Reproductive Health Matters 2004, 12 (24), pp. 138-153.
24 Niyongabo et al., "Burundi: Impact de dix années de guerre civile sur les endémo-épidémies."
25 Human Rights Watch/APRODH interview with Michèle N., Bujumbura, February 14, 2006. She was detained for about ten weeks after she was healed.
26 Human Rights Watch/APRODH interview with father of Noah B., Roi Khaled Hospital, Bujumbura, February 11, 2006.
27 Human Rights Watch/APRODH interview with Christine K., Prince Louis Rwagasore Clinic, Bujumbura, February 14, 2006.
28 Human Rights Watch/APRODH interview with nurse, Prince Régent Charles Hospital, Bujumbura, February 13, 2006; Human Rights Watch telephone interview with financial and administrative director, Roi Khaled Hospital, Bujumbura, April 2006.
29 Human Rights Watch/APRODH interview with social service worker, Ngozi Hospital, Ngozi, February 16, 2006.
30 Human Rights Watch/APRODH interview with Anne K., Bujumbura, February 14, 2006. She was detained for about one month after she got her bill.
31 Human Rights Watch/APRODH interview with Gabriel N., Roi Khaled Hospital, Bujumbura, February 11, 2006.
32 MSF, "Access to Health Care in Burundi," p. 6.
33 Christian Aid, "Servicing the Rich: How the EU will wreck the WTO talks," Case study 1: "Kenyan health warning," http://www.christian-aid.org.uk/indepth/512rich/Servicing percent20the percent20rich.pdf (accessed May 4, 2006).
34 "Ghana: Despite new health scheme, Babies detained in hospital pending payment", IRIN, September 16, 2005, http://www.irinnews.org/report.asp?ReportID=49114&SelectRegion=West_Africa&SelectCountry=GHANA (accessed August 11, 2006); "Ridge Hospital Detains Baby Over ¢3.2m", Public Agenda (Ghana), January 20, 2006, http://www.ghanaweb.com/public_agenda/issue.php?PUBLISHED=2006-01-20 (accessed August 11, 2006).
35 Initiative Congolaise pour la Justice et la Paix, "La 'détention' des femmes dans les milieux hospitaliers," March 8, 2006. Radio Okapi reported the same practice in Kamituga, South Kivu: "Plusieurs dizaines de femmes retenues à l'hôpital général de Kamituga," Radio Okapi, July 19, 2006.
36 "Maternity Charges Skyrocket", June 15, 2004, The Herald (Zimbabwe), www.allafrica.com/stories/200406150407.html (accessed February 12, 2006).
37 Hospitals often document the financial loss they incur, but usually do not document numbers of detained patients. Most statistics show how many bills have been left unpaid, and provide information on the cases of the patients, as well as about benefactors. Some hospitals also document the number of escapees. There is no standard breakdown that hospitals must follow, and statistics vary in detail and format.
38 Human Rights Watch/APRODH interview with director and other managers, Prince Louis Rwagasore Clinic, Bujumbura, February 14, 2006.
39 Figures obtained from hospital records.
40 See section X, below, on the dilemma of being a benefactor.
41 Data for the month of April are missing. Handwritten additions to the statistics of June 2005 have not been taken into account.
42 Data for the month of December are missing. The figure is based on lists of unpaid bills by escaped patients.
43 http://finance.yahoo.com/currency (accessed August 24, 2006)
44 According to records kept by the hospitals themselves. There is no standard format for the hospitals so the statistics vary in detail and format.
45 Unpaid bills by escaped patients, January-November 2005.
46 The hospital has kept statistics of indigent patients who were unable to pay their bill. However some settled them later, for example when they found benefactors.
47 See table 5. This figure is based on cases listed in three separate sections, gynecology/obstetrics, surgery, and operating theatre.
48 See below, section VIII.2, on exemption systems.
49 Human Rights Watch/APRODH interview with Christian B., Ngozi Hospital, Ngozi, February 16, 2006. It was unclear how long the period of detention – after he received the bill – was.
50 "Treatment Map Burundi," IRIN, January 2006, http://www.plusnews.org/AIDS/treatment/Burundi.asp (accessed August 1, 2006).
51 Numbers provided by "Progress on Global Access to Anti-Retroviral Therapy, A Report on "3 by 5" and Beyond" (WHO, 2006), p. 72, http://www.who.int/hiv/fullreport_en_highres.pdf (accessed July 27, 2006). The IRIN Treatment Map suggests a lower number of people are in need of antiretroviral treatment, about 25,000; however it is slightly older and probably based on older figures.
52 The original program was about $8 million. In May 2006 the Global Fund decided to give an additional $13 million for the fight against HIV/AIDS, http://www.theglobalfund.org/programs/search.aspx?lang=en (accessed May 18, 2006).
53 Multisectoral HIV/AIDS Control and Orphans Project – Burundi, http://web.worldbank.org/external/projects/main?pagePK=64283627&piPK=73230&theSitePK=343751&menuPK=343783&Projectid=P071371 (accessed July 26, 2006).
54 Human Rights Watch/APRODH interview with representative of an NGO assisting AIDS patients, Bujumbura, February 17, 2006.
55 There is however a special program for the treatment of tuberculosis, so some patients might not have to pay for such treatment. Human Rights Watch telephone interview with medical director in the Ministry Charged with the Fight against HIV/AIDS, Bujumbura, May 19, 2006.
56 Ibid. Earlier statistics point to similar figures. In 1995, an estimated 70 percent of in-patients at Prince Regent Hospital were HIV positive. See: Confronting AIDS: Public Priorities in a Global Epidemic, A World Bank Policy Research Report (Oxford University Press, 1997), http://www.worldbank.org/aidsecon/arv/conf-aids-4/ch4-1p2.htm (accessed May 18, 2006), table 4.4.
57 Human Rights Watch/APRODH interview with Spéciose N., Bujumbura, February 23, 2006.
58 The statistics of Prince Louis Rwagasore Clinic include some cases of indigents who could not pay initially, but eventually found a way to settle the bill.
59 See table 5.
60 Human Rights Watch/APRODH interview with guards, Prince Louis Rwagasore Clinic, Bujumbura, February 14, 2006.
61 WHO, "Burundi, Health Sector Needs Assessment."
62 L.P. Freedman, "Using human rights in maternal mortality programs: from analysis to strategy", International Journal of Gynecology & Obstetrics, vol. 75 (2001), pp. 51-60; Millennium Project, Task Force on Child Health and Maternal Health, "Who's got the power? Transforming health systems for women and children," http://www.unmillenniumproject.org/documents/maternalchild-complete.pdf (accessed July 31, 2006), pp. 5-6.
63 UNICEF, Burundi Statistics; WHO, "Heath Action in Crises – Burundi," http://www.who.int/hac/crises/bdi/background/Burundi_Dec05.pdf (accessed July 28, 2006); WHO, "Burundi, Health Sector Needs Assessment."
64 Millennium Project, Task Force on Child Health and Maternal Health, "Who's got the power?" pp. 5-6.
65 See section below on the government response.
66 As in many other countries, doctors in Burundi take an oath as the basis of their ethics. It is called the Geneva Declaration (Serment de Genève) and is a modern version of the Hippocratic Oath. Among other things, it says "The health of my patients will be my first consideration; ... I will not permit considerations of age, disease or disability, creed, ethnic origin, gender, nationality, political affiliation, race, sexual orientation, social standing or any other factor to intervene between my duty and my patient; ... I will not use my medical knowledge to violate human rights and civil liberties, even under threat." See English and French versions at http://www.wma.net/e/policy/c8.htm (accessed August 8, 2006).
67 Human Rights Watch/APRODH interview with Christine K., Prince Louis Rwagasore Clinic, Bujumbura, February 14, 2006.
68 Human Rights Watch/APRODH interview with Pierre B., Prince Régent Charles Hospital, Bujumbura, February 13, 2006.
69 Human Rights Watch/APRODH interview with Josephine C., Prince Régent Charles Hospital, Bujumbura, February 13, 2006.
70 Human Rights Watch/APRODH interview with Claudine N., Roi Khaled Hospital, Bujumbura, February 11, 2006.
71 Human Rights Watch/APRODH interview with Michèle N., Bujumbura, February 14, 2006; Unpublished document on hospital detention by international organization, August 2005. At Prince Régent Hospital detained patients are often moved to ward nine but are permitted to move about elsewhere in the building.
72 Human Rights Watch/APRODH interviews with Théodore N., Prince Régent Charles Hospital, Bujumbura, February 13, 2006; Michèle N., Bujumbura, February 14, 2006; Félicité G. and Valentine Z., Ngozi Hospital, Ngozi, February 15, 2006.
73 Human Rights Watch/APRODH interview with Amélie B., Roi Khaled Hospital, Bujumbura, February 11, 2006.
74 Human Rights Watch/APRODH interview with Théodore N., Prince Régent Charles Hospital, Bujumbura, February 13, 2006.
75 Human Rights Watch/APRODH interview with David S., Gitega Hospital, Gitega, February 16, 2006.
76 Human Rights Watch/APRODH interview with financial and administrative director, Ngozi Hospital, Ngozi, February 15, 2006.
77 Human Rights Watch/APRODH interview with Félicité G., Ngozi Hospital, Ngozi, February 15, 2006.
78 Human Rights Watch/APRODH interviews with Célestine H., Amélie B., Claudine N., Roi Khaled Hospital, Bujumbura, February 11, 2006. Human Rights Watch/APRODH interviews with Michèle N., Bujumbura, February 14, 2006.
79 Human Rights Watch/APRODH interview with financial and administrative director, Prince Régent Charles Hospital, Bujumbura, February 10, 2006.
80 Human Rights Watch/APRODH interview with Michèle N., Bujumbura, February 14, 2006.
81 Human Rights Watch/APRODH interview with Agnès I., Prince Louis Rwagasore Clinic, Bujumbura, February 14, 2006.
82 Human Rights Watch/APRODH interview with guards, Prince Louis Rwagasore Clinic, Bujumbura, February 14, 2006.
83 Human Rights Watch/APRODH interview with Félicité G., Ngozi Hospital, Ngozi, February 15, 2006.
84 Human Rights Watch/APRODH interview with David S., Gitega Hospital, Gitega, February 16, 2006.
85 Human Rights Watch/APRODH interviews with Agnès I. and Christine K., Prince Louis Rwagasore Clinic, Bujumbura, February 14, 2006.
86 Human Rights Watch/APRODH interview with Michèle N., Bujumbura, February 14, 2006.
87 Human Rights Watch/APRODH interview with Emérite N., Gitega Hospital, Gitega, February 16, 2006. Another woman reported the same refusal by nurses to remove the stitches in her incision. Human Rights Watch/APRODH interview with Berthilde N., Gitega Hospital, Gitega, February 16, 2006.
88 Human Rights Watch/APRODH interview with Dorothée H., Prince Régent Charles Hospital, Bujumbura, February 13, 2006.
89 Human Rights Watch/APRODH interview with Agnès I., Prince Louis Rwagasore Clinic, Bujumbura, February 14, 2006.
90 Human Rights Watch/APRODH interview with Amélie B., Roi Khaled Hospital, Bujumbura, February 11, 2006.
91 Human Rights Watch/APRODH interview with father of Noah B., Roi Khaled Hospital, Bujumbura, February 11, 2006.
92 APRODH interview with hospital staff, Bururi Hospital, Bururi, March 2006.
93 Human Rights Watch/APRODH interview with Christian B., Ngozi Hospital, Ngozi, February 16, 2006.
94 APRODH interviews with Régine K. and Joëlle N., Ngozi Hospital, Ngozi, March 15, 2006.
95 In this report, "child" refers to anyone under the age of eighteen. The UN Convention on the Rights of the Child, to which Burundi is a party, states: "For purposes of the present Convention, a child is every human being below the age of eighteen years unless under the law applicable to the child, majority is attained earlier."
96 Human Rights Watch/APRODH interview with grandmother of Mohamed S., Roi Khaled Hospital, Bujumbura, February 11, 2006.
97 Human Rights Watch/APRODH interview with father of Noah B., Roi Khaled Hospital, Bujumbura, February 11, 2006.
98 Human Rights Watch/APRODH interview with Noah B., Roi Khaled Hospital, Bujumbura, February 11, 2006. There are many reasons why children in Burundi may go to school later than the usual age for primary school, including insecurity during the war and the government's waiving of school fees during 2005.
99 Human Rights Watch/APRODH interview with Félix M., Prince Régent Charles Hospital, Bujumbura, February 13, 2006.
100 Human Rights Watch interview with Charles Atebawone, chief, Claims/Property Survey Unit, ONUB headquarters, Bujumbura, March 7, 2006.
101 Human Rights Watch interview with mother of Felix M., Bujumbura, May 11, 2006.
102 Human Rights Watch interview with Adèle A., Prince Régent Charles Hospital, Bujumbura, June 23, 2006.
103 Human Rights Watch/APRODH interview with nurse, Roi Khaled Hospital, Bujumbura, February 11, 2006.
104 Ibid.
105 Association Burundaise pour la Protection des Droits Humains et des Personnes Détenues, "Projet : secours aux indigents emprisonnés dans les hôpitaux," September 2005.
106 Save the Children, "The Cost of Coping with Illness," p. 3. The study was based on surveys done in households and at health facilities, focus group discussions, and interviews with key informants.
107 MSF, "Access to Health Care in Burundi," p .46.
108 Ibid.
109 Human Rights Watch/APRODH interview with Gabriel N., Roi Khaled Hospital, Bujumbura, February 11, 2006.
110 Human Rights Watch/APRODH interview with father of Noah B., Roi Khaled Hospital, Bujumbura, February 11, 2006.
111 Human Rights Watch/APRODH interview with Josephine C., Prince Régent Charles Hospital, Bujumbura, February 13, 2006.
112 Human Rights Watch/APRODH interview with Olivia N., Roi Khaled hospital, Bujumbura, February 11, 2006.
113 Human Rights Watch/APRODH interview with Gabriel N., Roi Khaled Hospital, Bujumbura, February 11, 2006.
114 Ibid.
115 Human Rights Watch/APRODH interview with Dr. Julien Kamyo, chef de cabinet, Ministry of Health, Bujumbura, February 13, 2006.
116 Human Rights Watch/APRODH interview with director and other managers, Prince Louis Rwagasore Clinic, Bujumbura, February 14, 2006.
117 Human Rights Watch/APRODH interview with director, Roi Khaled Hospital, Bujumbura, February 14, 2006.
118 Human Rights Watch/APRODH interviews with financial and administrative director, Prince Régent Charles Hospital, Bujumbura, February 10, and with administrator, Roi Khaled Hospital, Bujumbura, February 11, 2006.
119 Human Rights Watch/APRODH interview with Dr. Julien Kamyo, chef de cabinet, Ministry of Health, Bujumbura, February 13, 2006.
120 Human Rights Watch/APRODH interviews with Béatrice Ntahe, chef de cabinet, Ministry of National Solidarity, Human Rights and Gender, February 17; financial and administrative director, Ngozi Hospital, Ngozi, February 15; and financial and administrative director, Prince Régent Charles Hospital, Bujumbura, February 10, 2006.
121 "150 malades indigents libérés," Le Renouveau (Bujumbura), December 27, 2005.
122 Human Rights Watch interview with representative of the Ministry of National Solidarity, Human Rights and Gender, Bujumbura, May 10, 2006.
123 Human Rights Watch/APRODH interview with Béatrice Ntahe, chef de cabinet, Ministry of National Solidarity and Human Rights, February 17, 2006.
124 Human Rights Watch/APRODH interview with Dr. Julien Kamyo, chef de cabinet, Ministry of Health, Bujumbura, February 13, 2006; République du Burundi, Ministère de la Santé, "Plan national de développement sanitaire 2006-2010." There are other insurances for state employees and private business.
125 Save the Children, "The Cost of Coping with Illness,"p. 1.
126 République du Burundi, Ministère de la Santé, "Plan national de développement sanitaire 2006-2010," p. 28.
127 MSF, "Access to Health Care in Burundi," p. 49.
128 Human Rights Watch/APRODH interview with Claudine N., Roi Khaled Hospital, Bujumbura, February 11, 2006.
129 Human Rights Watch/APRODH interviews with financial and administrative director, Roi Khaled Hospital, Bujumbura, February 14, and Dorothée H., Prince Régent Charles Hospital, Bujumbura, February 13, 2006.
130 Human Rights Watch/APRODH interview with director, Prince Louis Rwagosore Clinic, Bujumbura, February 14, 2006.
131 Human Rights Watch/APRODH interviews with financial and administrative director, Ngozi Hospital, Ngozi, February 15, and financial and administrative director, Gitega Hospital, Gitega, February 16, 2006.
132 Human Rights Watch/APRODH interviews with Emérite N. and Berthilde N., Gitega Hospital, Gitega, February 16, 2006.
133 MSF, "Access to Health Care in Burundi," p. 49. Save the Children, "The Cost of Coping with Illness,"p. 3. Some interviewees in the Save the Children study alleged that people had obtained indigence cards through bribery rather than based on the official criteria.
134 Human Rights Watch interview with local administrator, Bujumbura-rural province, April 7, 2006.
135 République du Burundi, Ministère de la Santé, "Plan national de développement sanitaire 2006-2010."
136 Save the Children, "The Cost of Coping with Illness," p. 3.
137 Human Rights Watch/APRODH interview with Christian B., Ngozi Hospital, Ngozi, February 16, 2006.
138 Human Rights Watch/APRODH interview with Désirée N., Roi Khaled Hospital, Bujumbura, February 11, 2006.
139 Human Rights Watch interview with director, Roi Khaled Hospital, Bujumbura, February 14, 2006.
140 Human Rights Watch/APRODH interview with nurse, Roi Khaled Hospital, Bujumbura, February 11, 2006.
141 Human Rights Watch/APRODH interview with financial and administrative director, Prince Régent Hospital, Bujumbura, February 10, 2006.
142 The Accord used the term Sinistré for Displacedin its French and English versions. The word has been translated here for clarity.
143 Arusha Peace and Reconciliation Agreement for Burundi, Protocol IV. The accord also foresaw the creation of a National Fund for Sinistrés. It further stated that "The Government shall ensure, through special assistance, the protection, rehabilitation and advancement of vulnerable groups, namely child heads of families, orphans, street children, unaccompanied minors, traumatized children, widows, women heads of families, juvenile delinquents, the physically and mentally disabled, etc." http://www.usip.org/library/pa/burundi/pa_burundi_08282000_pr4ch1.html, (accessed on April 25, 2006).
144 The Fund was financed through the operating budget of the CNRS, the Social and Cultural Fund (which had been previously under the domain of the Ministry of National Solidarity, Human Rights and Gender), UNHCR, and a World Bank project called Credit de Relance Economique. Human Rights Watch interview with Claire Nzeyimana, Volet Affaires Financières et Mobilisation des Fonds, CNRS, May 9, 2006.
145 Human Rights Watch interview with local administrator, Bujumbura-rural province, April 7, 2006.
146 Human Rights Watch interview with representative of PARESI, May 8, 2006.
147 Human Rights Watch/APRODH interview with Dorothée H., Prince Régent Charles Hospital, Bujumbura, February 13, 2006.
148 The three hospitals were Prince Régent Charles Hospital, Roi Khaled Hospital and CMCC Djabe. Human Rights Watch interview with Claire Nzeyimana, Volet Affaires Financières et Mobilisation des Fonds, CNRS, May 9, 2006.
149 On corruption, see section below on transparency. Human Rights Watch interviews with representative of PARESI, Bujumbura, May 8, and with Claire Nzeyimana, Volet Affaires Financières et Mobilisation des Fonds, CNRS, Bujumbura, May 9, 2006.
150 Human Rights Watch interview with Béatrice Ntahe, chef de cabinet, Ministry of National Solidarity, Human Rights and Gender, February 17, 2006.
151 Human Rights Watch interview with representative of the Ministry of National Solidarity, Human Rights and Gender, Bujumbura, May 10, 2006. When we asked the chef de cabinet to explain the use of the funds, she refused to do so: Human Rights Watch interview with Béatrice Ntahe, chef de cabinet, Ministry of National Solidarity, Human Rights and Gender, February 17, 2006.
152 APRODH interviews with financial and administrative director, Muyinga Hospital, Muyinga, March 6, and with chief accountant, Matana Hospital, Matana, March 8, 2006.
153 APRODH interview with financial and administrative director, Muyinga Hospital, Muyinga, March 6, 2006.
154 MSF, "Access to Health Care in Burundi," p. 46.
155 Human Rights Watch/APRODH interview with director and financial and administrative director, Prince Louis Rwagosore Clinic, Bujumbura, February 14, 2006.
156 MSF, "Access to Health Care in Burundi," pp. 10-12.
157 APRODH interview with financial and administrative director and with nurse, Buhiga Hospital, Karuzi, March 7, 2006. Such models might be easier to practice in smaller hospitals where there are less complex and expensive cases of treatment – those are often sent to the capital.
158 APRODH interview with director, Rumonge Hospital, Rumonge, March 1, 2006.
159 "Burundi: Nkurunziza announces free maternal healthcare, pay rise for workers", IRIN, May 1, 2006, http://www.irinnews.org/report.asp?ReportID=53075&SelectRegion=Great_Lakes (accessed May 3, 2006).
160 UNICEF, "Burundi: Free primary education for all children," September 7, 2006, http://www.unicef.org/infobycountry/burundi_28197.html (accessed July 3, 2006).
161 République du Burundi, Ministère de la Santé, "Plan national de développement sanitaire 2006-2010," pp. 35-46. The health plan also made other, broader recommendations. See section 5 in this chapter.
162 According to the Ministry of Health, the reform aims to reduce infant and maternal mortality in Burundi. Human Rights Watch telephone interview with chef de cabinet, Ministry of Health, Bujumbura, June 22, 2006.
163 Human Rights Watch telephone interview with financial and administrative director, Prince Louis Rwangasore Clinic, Bujumbura, June 19, 2006.
164 Human Rights Watch telephone interview with diplomat in Bujumbura, June 19, 2006.
165 Human Rights Watch telephone interview with World Bank official, Washington D.C., March 31, 2006.
166 Human Rights Watch telephone interview with financial and administative director, Prince Louis Rwangasore Clinic, Bujumbura, June 19, 2006.
167 "Burundi: Side effects of free maternal, child health care", IRIN, June 9, 2006. http://www.irinnews.org/report.asp?ReportID=53836 (accessed July 3, 2006).
168 Announcement on Radio Isanganiro, May 10, 2006.
169 Human Rights Watch telephone interview with financial and administrative director, Roi Khaled Hospital, Bujumbura, June 20, 2006.
170 Announcement on Radio Bonesha, May 22, 2006.
171 "Burundi: Side effects of free maternal, child health care", IRIN.
172 Human Rights Watch telephone interview with financial and administrative director, Prince Louis Rwangasore Clinic, Bujumbura, July 27, 2006. Medicine for children under five and women giving birth is paid for at health centers.
173 Human Rights Watch telephone interview with financial and administative director, Prince Louis Rwangasore Clinic, Bujumbura, June 19, 2006.
174 Human Rights Watch telephone interview with Dr. Julien Kamyo, chef de cabinet, Ministry of Health, June 22, 2006.
175 Human Rights Watch telephone interview with Belgian official, June 21, 2006. This was echoed by other diplomats and donors.
176 Figures provided by donor government, Human Rights Watch telephone interview, June 19, 2006.
177 Of $10 million, 14 percent went to the central level, 23 percent went to the intermediate level and 63 percent went to the operational level – that is, essential medicines, vaccinations, contracts, and essential health care for deliveries and children. The $3 million is part of the funds allocated to the operational level.
178 Human Rights Watch telephone interview with Dr. Julien Kamyo, chef de cabinet, Ministry of Health, June 22, 2006.
179 Human Rights Watch telephone interview with Dr. Julien Kamyo, chef de cabinet, Ministry of Health, August 8, 2006.
180 Human Rights Watch interview with social worker, Roi Khaled Hospital, Bujumbura, June 23, 2006; Human Rights Watch telephone interview with financial and administrative director, Prince Louis Rwangasore Clinic, Bujumbura, June 19, 2006.
181 Human Rights Watch interviews with financial and administrative directors, Prince Louis Rwangasore Clinic and Roi Khaled Hospital, Bujumbura, August 8, 2006.
182 ICESCR, article 12(2)(a).
183 Human Rights Watch interview with head of accounting, Roi Khaled Hospital, Bujumbura, June 23, 2006.
184 Human Rights Watch interviews with staff at Roi Khaled and Prince Régent Charles Hospitals, June 23, 2006.
185 Human Rights Watch telephone interview with financial and administative director, Prince Louis Rwangasore Clinic, Bujumbura, June 19, 2006.
186 Human Rights Watch interview with Jerôme N., Roi Khaled Hospital, Bujumbura, June 23, 2006.
187 Human Rights Watch interview with Augustin M., Prince Régent Charles Hospital, Bujumbura, June 23, 2006.
188 Human Rights Watch interviews with Jerôme N., Roi Khaled Hospital, Bujumbura, June 23, and with Augustin M. and Adèle A., Prince Régent Charles Hospital, Bujumbura, June 23, 2006.
189 Human Rights Watch/APRODH interview with Dr. Julien Kamyo, chef de cabinet, Ministry of Health, Bujumbura, February 13, 2006.
190 Abuja Declaration on HIV/AIDS, Tuberculosis and Other Related Infectious Diseases, http://www.uneca.org/ADF2000/Abuja%20Declaration.htm (accessed July 31, 2006).
191 République du Burundi, Ministère de la Santé, "Plan national de développement sanitaire 2006-2010," pp. 48-49.
192 Ibid.
193 Human Rights Watch/APRODH interview with Dr. Julien Kamyo, chef de cabinet, Ministry of Health, Bujumbura, February 13, 2006.
194 République du Burundi, "Cadre Stratégique de Croissance et de Lutte contre la Pauvreté," July 2006, p. 59.
195 Human Rights Watch/APRODH interview with financial and administrative director, Prince Régent Charles Hospital, Bujumbura, February 10, 2006.
196 Human Rights Watch/APRODH interview with financial and administrative director, Ngozi Hospital, Ngozi, February 15. Similar information was provided by the financial and administrative directors of Roi Khaled and Prince Régent Charles Hospitals.
197 Human Rights Watch/APRODH interview with Dr. Julien Kamyo, chef de cabinet, Ministry of Health, Bujumbura, February 13, 2006.
198 Human Rights Watch/APRODH interview with director and other managers, Prince Louis Rwagasore Clinic, Bujumbura, February 14, 2006.
199 Human Rights Watch/APRODH interview with financial and administrative director, Prince Régent Charles Hospital, Bujumbura, February 10, 2006.
200 République du Burundi, Ministère de la Santé, "Plan national de développement sanitaire 2006-2010," p. 26. This sum includes a housing allowance. On the situation of medical staff, see also Niyongabo et al., "Burundi: Impact de dix années de guerre civile sur les endémo-épidémies."
201 Human Rights Watch interview with Claire Nzeyimana, Volet Affaires Financières et Mobilisation des Fonds, CNRS, May 9, 2006.
202 Human Rights Watch interview with representative of the Ministry of National Solidarity, Human Rights and Gender, Bujumbura, May 10, 2006.
203 Human Rights Watch interview with humanitarian agency, Bujumbura, February 12, 2006.
204 Radio Bonesha, February 24, 2006.
205 "Gitega – Santé: Les principaux facteurs qui freinent encore l'accessibilité aux soins de santé," Agence Burundaise de Presse, April 21, 2006.
206 Letter from Claude Beke Dassys, Ambassador of Côte d'Ivoire to the United Nations, Geneva, to President Laurent Gbagbo, September 2002; Human Rights Watch interview with Alexis Sinduhije, Bujumbura, May 10, 2006; "Burundi Court Convicts Killers of WHO Official", Mail & Guardian Online, May 4, 2005, http://www.mg.co.za/articlePage.aspx?area=/breaking_news/breaking_news__africa/&articleId=237024 (accessed April 29, 2006); "Burundi police killed aid worker," BBC News Online, May 4, 2005, http://news.bbc.co.uk/2/hi/africa/4512263.stm (accessed April 29, 2006); " Entrevue avec Me Bernard Maingain, membre du barreau de Bruxelles, avocat et conseiller de la partie civile dans l'affaire Kassy Manlan", Burundi news, June 6, 2005, http://burundi.news.free.fr/interviewavocat.html (accessed April 29, 2006).
207 "Burundi/Assemblée Nationale : Pas de quorum pour voter la loi portant création de la Brigade anti-corruption," Burundi Réalités, July 23, 2006, http://www.burundirealite.org/burundi/display_news_f.cfm?loc=1802 (accessed July 31, 2006); "Burundi-politique : La grogne s'intensifie à l'Assemblée Nationale au sein des députés du FRODEBU, de l'UPRONA et du CNDD de Nyangoma" Burundi Express, July 13, 2006, http://www.burundiexpress.org/article.php3?id_article=128 (accessed August 8, 2006). Critics maintained the proposed anti-corruption brigade will be a police body, separate from the ordinary police. However the constitution stipulates that there can only be one national police force.
209 Millennium Project, Task Force on Child Health and Maternal Health, "Who's got the power?" p. 15.
210 The 2002 Monterrey Conference was the United Nations International Conference on Financing for Development where donors pledged to support the Millennium Development Goals.
211 Millennium Project, "The 0.7% Target: An In-Depth Look," http://www.unmillenniumproject.org/involved/action07.htm (accessed August 1, 2006).
212 International Crisis Group, "A Framework for Responsible Aid to Burundi," February 2003, http://www.crisisgroup.org/library/documents/report_archive/A400901_21022003.pdf (accessed May 3, 2006).
213 "Burundi: Donors pledge U.S .$170 million for post-war recovery bid," IRIN, http://www.irinnews.org/report.asp?ReportID=51969&SelectRegion=Great_Lakes (accessed May 3, 2006).
214 République du Burundi, "Cadre Stratégique de Croissance et de Lutte contre la Pauvreté."
215 Délégation de la Commission Européenne au Burundi, "La Commission Européenne au Burundi," February 1, 2006.
216 USAID, "Budget Burundi,"http://www.usaid.gov/policy/budget/cbj2006/afr/bi.html (accessed May 3, 2006).
217 €9.5 million are newly committed funds, €35 million were from previous commitments. Human Rights Watch telephone interview with Bundesministerium für Wirtschaftliche Zusammenarbeit, May 3, 2006.
218 Human Rights Watch telephone interview with DFID Burundi, May 3, 2006.
219 International Monetary Fund, Burundi: Enhanced Initiative for Heavily Indebted Poor Countries – Decision Point Document (Washington D.C.: IMF, 2005), http://siteresources.worldbank.org/INTDEBTDEPT/DecisionPointDocuments/20645009/cr05329.PDF (accessed August 1, 2006), p. 25 (box 7: Expenditure Priorities for the Use of HIPC Debt Relief).
220 Human Rights Watch telephone interview with World Bank official, March 31, 2006; "Burundi: IMF and World Bank Support U.S.$1.5 Billion in Debt Service Relief For Burundi," World Bank news release, http://web.worldbank.org/WBSITE/EXTERNAL/COUNTRIES/AFRICAEXT/BURUNDIEXTN/0,,contentMDK:20606461~menuPK:343757~pagePK:141137~piPK:141127~theSitePK:343751,00.html (accessed May 3, 2006).
221 Letter from Athanase Gahungu, minister of finance, and Salvator Toyi, governor of the Bank of Burundi, to Rodrigo Rato, managing director of the International Monetary Fund, June 30, 2005.
222 See Manfred Nowak, U.N. Covenant on Civil and Political Rights: CCPR Commentary (N.P. Engel, 1993), pp. 172-73.
223 Nowak, U.N. Covenant on Civil and Political Rights, pp. 193-96. This provision does not apply to criminal offenses related to debts such as fraud and failure to pay maintenance.
224 General Comment No. 21. Forty-fourth session, 1992, http://www.unhchr.ch/tbs/doc.nsf/(Symbol)/3327552b9511fb98c12563ed004cbe59?Opendocument (accessed May 11, 2006).
225 ICESCR, Article 12.1.
226 Article 12.2.
227 UN Committee on Economic, Social and Cultural Rights, "Substantive Issues Arising in the Implementation of the International Covenant on Economic, Social and Cultural Rights," General Comment No. 14 (2000). The right to the highest attainable standard of health (article 12 of the International Covenant on Economic, Social and Cultural Rights), http://www.unhchr.ch/tbs/doc.nsf/(Symbol)/40d009901358b0e2c1256915005090be?Opendocument (accessed May 11, 2006)
228 UN Committee on Economic, Social and Cultural Rights, General Comment No.14.
229 Ibid. The UN special rapporteur on the right of everyone to the enjoyment of the highest attainable standards of physical and mental health, Paul Hunt, has developed some indicators to measure progress with regard to the realization of the right to health. Commission on Human Rights, "Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standards of physical and mental health," E/CN.4/2006/48, March 3, 2006; "The Right to Health: An Interview with Professor Paul Hunt", Essex Human Rights Review, vol. 2, no. 1, http://projects.essex.ac.uk/ehrr/archive/pdf/File4-Hunt.pdf (accessed May 12, 2006).
230 Article 12.2. (a): "The steps to be taken by the States Parties to the present Covenant to achieve the full realization of this right shall include those necessary for: (a) The provision for the reduction of the stillbirth-rate and of infant mortality and for the healthy development of the child." According to the UN Committee on Economic, Social and Cultural Rights, this means to "improve child and maternal health, sexual and reproductive health services" generally, including access to family planning, pre- and post-natal care, emergency obstetric services and access to information, as well as to resources necessary to act on that information. UN Committee on Economic, Social and Cultural Rights, General Comment No. 14.
231 Convention on the Rights of the Child (CRC), Article 24. Burundi ratified the CRC in 1990. The African Charter on the Rights and Welfare of the Child contains similar provisions, though Burundi has not ratified it.
232 Convention on the Elimination of All Forms of Discrimination against Women (CEDAW), Article 12. Burundi ratified CEDAW in 1992. The Committee on the Elimination of Discrimination against Women issued General Recommendation No. 24 on women and health, stating that "Many women are at risk of death or disability from pregnancy-related causes because they lack the funds to obtain or access the necessary services, which include ante-natal, maternity and post-natal services. The Committee notes that it is the duty of States parties to ensure women's right to safe motherhood and emergency obstetric services and they should allocate to these services the maximum extent of available resources."

